Annual Summary of Disease Activity:
Disease Control Newsletter (DCN)
Related Topics
Contact Info
HIV Infection and AIDS, 2019
HIV/AIDS incidence in Minnesota remains moderately low. In 2018, state-specific HIV infection rates ranged from 2.5 per 100,000 population in Wyoming to 28.6 per 100,000 in Georgia. Minnesota had the 14th lowest rate (6.2 cases per 100,000 population). In 2018, state-specific AIDS diagnosis rates ranged from 0.3 per 100,000 persons in Wyoming to 11.6 per 100,000 population in Georgia. Minnesota had the 15th lowest rate (2.1 cases per 100,000 population).
As of December 31, 2019, 2,112 cases of HIV infection (2,308 AIDS at first diagnosis, and 9,804 HIV [non-AIDS] cases) were reported among Minnesota residents. By the end of 2019, an estimated 9,193 persons with HIV/AIDS were living in Minnesota.
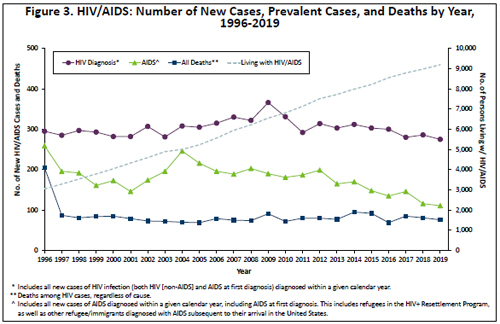
The annual number of AIDS cases reported in Minnesota increased steadily from 1982 through the early 1990s, reaching a peak of 361 cases in 1992. Beginning in 1996, the annual number of new AIDS diagnoses and deaths declined sharply, primarily due to better antiretroviral therapies. In 2019, 111 new AIDS cases (Figure 3) and 76 deaths among persons living with HIV infection in Minnesota were reported.
The number of HIV (non-AIDS) diagnoses has varied over the past decade. There was a peak of 278 newly diagnosed HIV (non-AIDS) cases in 2009, and a low of 215 new HIV (non- AIDS) cases reported in 2017, which is slightly lower than 219 cases reported in 2019.
In 2019, 81% (222/275) of new HIV diagnoses (both HIV [non-AIDS] and AIDS at first diagnosis) occurred in the metropolitan area. In greater Minnesota there were 52 cases in 31 of 78 counties. HIV infection is most common in areas with higher population densities and greater poverty.
The majority of new HIV infections in Minnesota occur among males. Trends in the annual number of new HIV infections diagnosed among males differ by race/ethnicity. New infections occurred primarily among white males in the 1980s and early 1990s. Whites still comprise the largest number of HIV infections among males, but the proportion of cases that white males account for is decreasing. In 2019, there were 84 new infections among white males, which is slightly less than half of new HIV infections among males (42%). Among black African American males, there were 51 new HIV diagnoses in 2019, which is about a quarter of new HIV infections among males (26%). Among Hispanic males of any race and black African-born males, there were 33 and 12 new HIV infections in 2019 respectively.
Females account for an increasing percentage of new HIV infections, from 11% of new infections in 1990 to 28% in 2019. Trends in HIV infections diagnosed annually among females also differ by race/ethnicity. Early in the epidemic, whites accounted for the majority of newly diagnosed infections. Since 1991, the number of new infections among women of color has exceeded that of white women.
In 2019, women of color accounted for 68% of new HIV infections among females in Minnesota. The number of diagnoses among African-born women has been increasing over the past decade. In 2019, the number of new cases among African-born women was 25, accounting for 33% of all new diagnoses among women. In 2019, there were 11 cases (14%) diagnosed among African American women.
Despite relatively small numbers of cases, HIV/AIDS affects persons of color disproportionately in Minnesota. In 2019, men of color comprised approximately 17% of the male population in Minnesota and 58% of new HIV diagnoses among men. Similarly, persons of color comprised approximately 13% of the female population in Minnesota and 68% of new HIV infections among women. The use of race can be a proxy for other risk factors, including lower socioeconomic status and education, and race is not considered a biological cause of disparities in the occurrence of HIV.
Historically, race/ethnicity data for HIV/AIDS in Minnesota have grouped non-African born blacks and black African-born persons together as “black.” In 2001, MDH began analyzing these groups separately, and a marked trend of increasing numbers of new HIV infections among black African-born persons was observed. In 2019, there were 37 new HIV infections reported among black Africans. While black African-born persons comprise less than 1% of the state’s population, they accounted for 14% of all HIV infections diagnosed in Minnesota in 2019.
In 2019, there were 111 diagnosed with HIV <30 years of age, accounting for 40% of all cases. Most of the cases were among young males where 82% of cases <30 years were male.
Since the beginning of the epidemic, male-to-male sex (men who have sex with men; MSM) has been the predominant mode of exposure to HIV reported in Minnesota. In 2019, MSM (including MSM who also inject drugs) accounted for 67% of new diagnoses among men. Heterosexual contact with a partner who has or is at increased risk of HIV infection is the predominant mode of exposure to HIV for women.
In the fall of 2019, an outbreak was declared among persons who inject drugs (PWID) diagnosed with HIV in Minnesota. Statewide there was a two-fold increase among PWID with 11 cases in 2018 increasing to 22 cases in 2019. The outbreak area includes residents of Hennepin and Ramsey counties where about three quarters of the statewide cases are located (16, 72%). Persons likely to be at high risk for HIV infection include sex partners or syringe-sharing partners of people known to be living with HIV, PWID and their sex partners and needle sharing partners, persons who exchange sex for income or other items they need, and persons who experienced or are currently experiencing homelessness.
HIV perinatal transmission in the United States decreased 90% since the early 1990s. The trend in Minnesota has been similar. While the number of births to HIV-infected women increased nearly 7-fold between 1990 and 2018, with 57 births to pregnant persons in 2019, the rate of perinatal transmission decreased, from 15% in 1994-1996 to 0.6% over the last 3 years (2017-2019), with 1 HIV-positive birth in 2017.
- Find up to date information at>> HIV (HIV/AIDS)
- Full issue>> Annual Summary of Communicable Diseases Reported to the Minnesota Department of Health, 2019