Center of Excellence in Newcomer Health
- Minnesota Center of Excellence in Newcomer Health Home
- About
- Clinical Guidance and Clinical Decision Tools
- Health Education
- Publications and Presentations
- Trainings
- Newcomer Health Profiles
Spotlight
- Haitian Clinical Guidance
- OB-GYN Care for Afghans: A Toolkit for Clinicians
- Immigrant Health Matters
- Newcomer Education for Wellness Video Series
- MNCOE Connect
Related Topics
Burmese Refugee Health Profile
 Last updated: March 2024
Last updated: March 2024
On this page:
Priority health conditions
Background
Population movements
Health care access and conditions in refugee camps/urban settings
Medical screening of U.S.-bound refugees
Health conditions to consider in post-arrival medical screening
Summary
References
Priority health conditions
Available data indicate that the health conditions listed below are priority health conditions that healthcare providers should consider when caring for or assisting Burmese refugees. These conditions are considered more prevalent among this population.
Background
The Republic of the Union of Myanmar (formerly Burma) is located in Southeast Asia and shares borders with Bangladesh, India, China, Laos, and Thailand. Myanmar was granted independence from Britain in 1948, following the drafting of a constitution in 1947 [1]. In 1962, a military coup abolished the constitution and established a military junta, which is a group of military officers who rule the country after seizing power [1]. In 1990, the country held democratic elections, in which the main opposition party won a majority of votes. The military government however, refused to recognize the results and placed the opposition leaders under house arrest. Myanmar is currently undergoing a new democratic transition, with opposition parties being allowed to participate in elections and the military taking a less-active role in politics [1].
Myanmar is an ethnically diverse country. There are eight main ethnic groups inhabiting the country, with 130 distinctive subgroups. Of the estimated population of 56 million, the largest ethnic group, the Burmese, comprises about 68% of the population [2]. Other ethnic groups mostly occupy territories in the various border regions, including the Chin, Kachin, Karen, Mon, Rakhine, Shan, and Wa.
Figure 1: Location of Myanmar, Thailand, and Malaysia
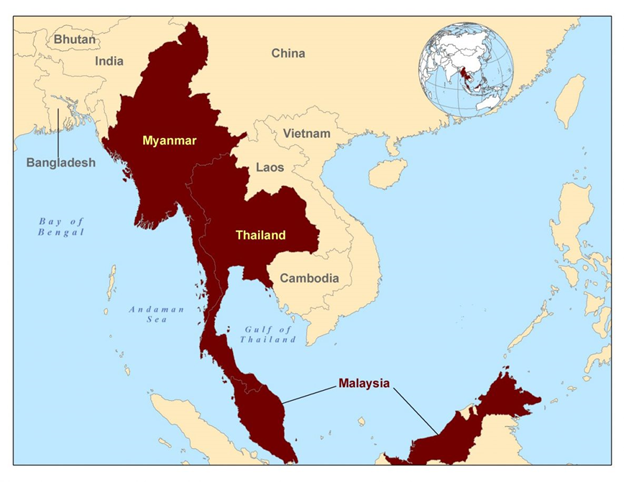
Source: Division of Global Migration and Quarantine (DGMQ), CDC
Compared to American culture, the Burmese are considerably more collectively oriented and less direct in communication [3]. Limitation of self-expression can reinforce collective values and identities and preserve harmony within the group, but also may lead to misinformation and poor communication with healthcare providers [3]. Providers should be aware that the politeness and modesty exhibited by the Burmese can lead to occasional misunderstandings [4]. Many Burmese refugees will require assistance from language interpreters during doctor visits due to language barriers. Culturally competent providers will also recognize that body language is important with Burmese refugees. There are varying body language taboos between minority groups in the Burmese population that may include concerns about touching other people, sitting higher than an elder, or pointing at others with fingers, hands or feet, etc. [5]
For more information about the orientation, resettlement, and adjustment of Burmese refugees, visit EthnoMed: Other Cultures - Burmese.
Population movements
Refugees from Myanmar are housed in camps in Thailand or urban settlements in Malaysia. Refugee camps in Thailand are located along Thailand’s border with Myanmar, while refugees in Malaysia reside mostly in Kuala Lumpur (Figure 2). The majority of refugees from Myanmar are from the various minority ethnic groups within the country, such as the Chin, Kachin, Karen, Mon, Rakhine, Shan, and Wa.
Figure 2. Location and size of Burmese refugee camps in Thailand (December, 2013)
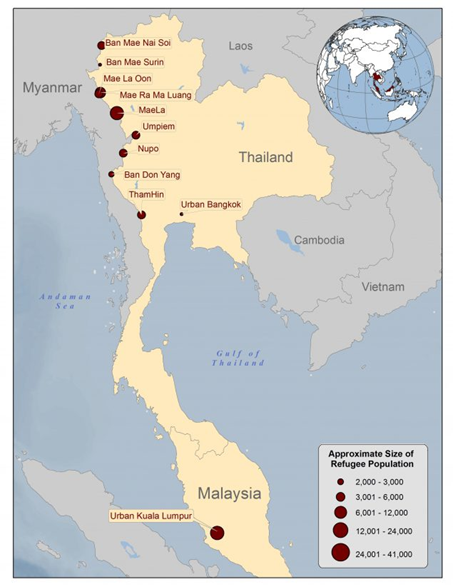
Source: Asia Team, DGMQ, CDC
Refugees from Myanmar began resettling into the United States in large numbers around 2008. From 2008-2014, approximately 109,000 Burmese refugees arrived in the United States from camps and urban settings in Thailand and Malaysia (Figure 3). Burmese refugees were mostly resettled from refugee camps in Thailand in the past, but are now increasingly being resettled from urban settings in Malaysia. Burmese refugees have also been resettled from countries other than Malaysia and Thailand.
Figure 3: Burmese refugee arrivals to the United States from Malaysia and Thailand, 2008-2014 (N=109,033)
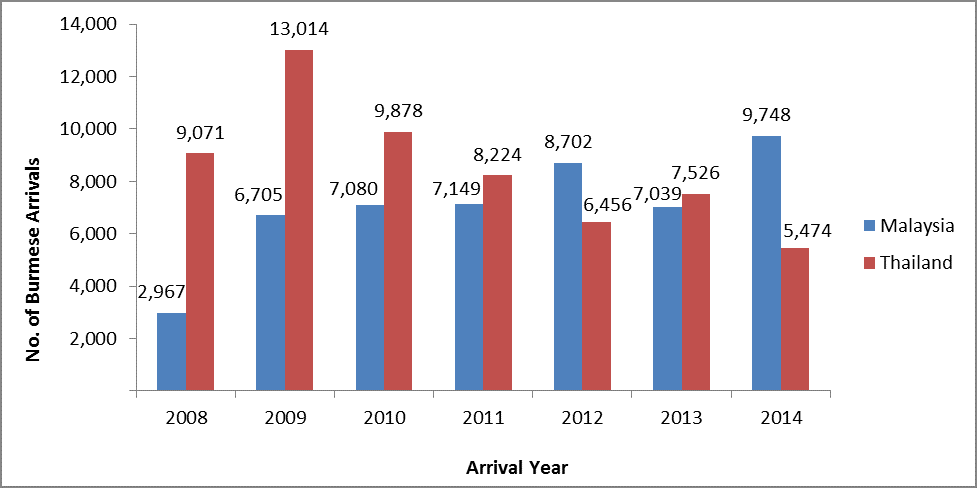
Source: U.S. Department of State, Bureau of Population, Refugees, and Migration (PRM), Worldwide Refugee Admissions Processing System (WRAPS)
From 2007-2023, nearly 185,000 refugees from Burma were resettled in the United States (Figure 4). The majority of refugees from Burma have been resettled from Thailand and Malaysia, with smaller numbers from other countries of asylum. The majority of refugees from Burma have been resettled to 10 states (Figure 5).
Figure 4: Refugee arrivals to the United States from Burma, 2007-2023 (N=184,487)
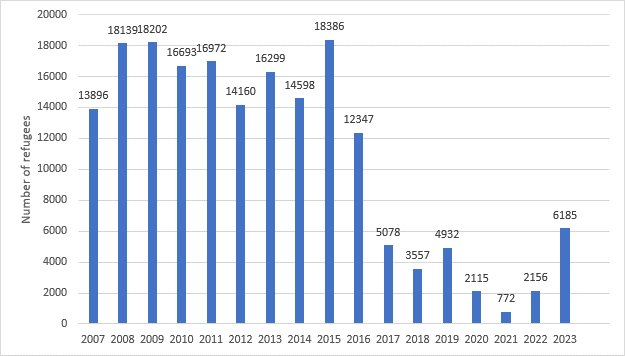
Figure 5: States of primary resettlement for all Burmese refugees, 2008-2014 (N=117,433)
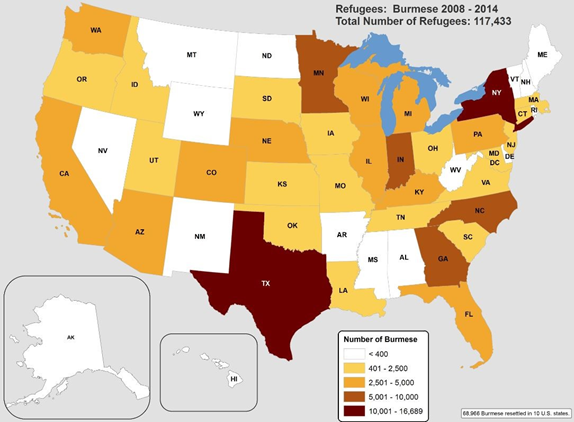
Table 1: Top 10 States of primary resettlement for Burmese refugees
| Top 10 States* | Number | Percent (%) |
|---|---|---|
| Texas | 16,689 | (14.2) |
| New York | 10,300 | (8.7) |
| Indiana | 8,216 | (7.0) |
| North Carolina | 6,386 | (5.4) |
| Georgia | 5,800 | (4.9) |
| Minnesota | 5,354 | (4.6) |
| Illinois | 4,632 | (3.9) |
| Washington | 4,069 | (3.5) |
| Arizona | 3,777 | (3.2) |
| Michigan | 3,743 | (3.2) |
*The remaining 40,067 refugees resettled to 39 other states.
Source: WRAPS
Refugees from Burma who are resettled into the United States are predominantly between the ages of 15-44 years (Figure 6)
Figure 6: Age distribution for Burmese refugees resettled to the United States, 2008-2014 (N=117,433)
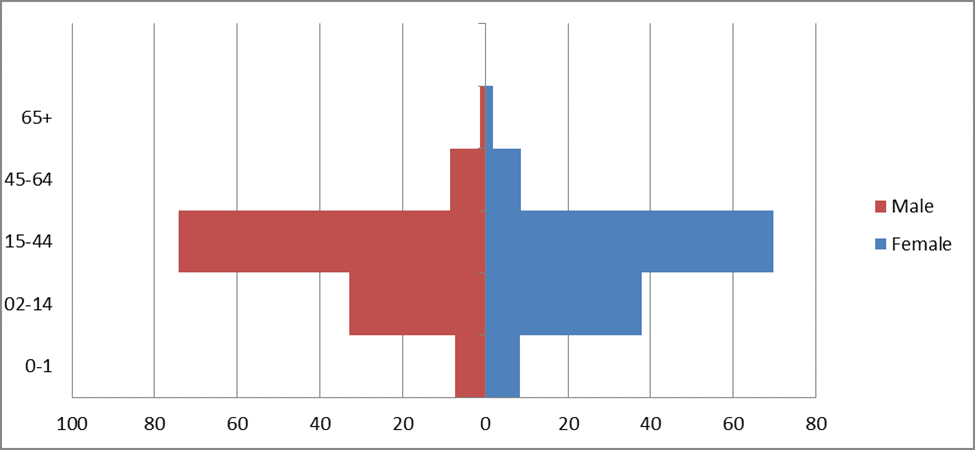
Source: Electronic Disease Notification System (EDN)
Health care access and conditions in refugee camps/urban settings
In Burmese refugee camps in Thailand, an average of 2.1% of children were found with acute malnutrition (wasting) [6]. Wasting malnutrition rates in camps are lower than in Thailand or Myanmar as a whole. An average of 40.8% (range 24.8%-49.7% in nine camps) of children surveyed were found with chronic malnutrition (stunting) [6]. Stunting malnutrition rates in the camps are higher than in Thailand and comparable to rates in Myanmar [6].
In 2014, the CDC field office in Thailand estimated immunization rates in refugee camps in Thailand for children less than 1 year of age were: Bacillus Calmette-Guérin (BCG) 88.3%, Polio 90%, and Diphtheria-Pertussis-Tetanus (DPT) 93.1%.
The following data are estimates from Burmese refugees in refugee camps in Thailand from January-December 2014.
Table 2. Reproductive health and gender-based violence metrics among refugees from Burma living in refugee camps in Thailand (2014)
| Antenatal Care | |
|---|---|
| Proportion of first time ANC visits made < 1st trimester | 46% |
| Coverage of syphilis screening in pregnancy | 68% |
| Prevalence of syphilis (ANC) | 0.8% |
| Abortion complication ratio* | 67.7 |
| Coverage of complete antenatal care | 97% |
| Coverage of antenatal tetanus immunization | 97% |
ANC=antenatal care
*number of live births/1000/month
| Delivery Care | |
|---|---|
| Total number of live births | 2,793 |
| Crude birth rate* | 1.9 |
| Proportion of all births attended by skilled health worker (excl. TBA) | 93% |
| Proportion of deliveries at health facility | 92% |
| Total number of still births | 28 |
| Stillbirth rate** | 9.9 |
| Proportion of low birth weight deliveries | 9% |
| Proportion of obstetric complications treated in health facilities*** | 99% |
| Proportion of all births performed by caesarean section | 6% |
TBA=traditional birth attendant
*number of live births/1000/month
**number of still births/1000 total (live and still) births
***number of obstetric complications/1000/month
| Postnatal care | |
|---|---|
| Coverage of complete postnatal care | 79% |
| Family Planning | |
|---|---|
| Contraceptive Prevalence Rate | 42% |
| Sexual and Gender-based Violence (SGBV) | |
|---|---|
| Total number of rape survivors seen in health center | 14 |
| Incidence of reported rape* | 1.1 |
| Proportion of rape survivors who receive PEP < 72 hrs | 0% |
| Proportion of female rape survivors who receive ECP < 120 hrs | 13% |
| Proportion of rape survivors who receive STI presumptive treatment < 2 wks | 17% |
PEP=post-exposure prophylaxis
ECP=Emergency Contraceptive Pill
****number of rapes / 10,000 / year
Source: CDC field office in Thailand
Medical screening of U.S.-bound refugees
All refugees who have been identified for resettlement to the United States receive medical assessments (Figure 7). Some assessments occur several months before departure and some occur immediately before departure to the United States.
Figure 7: Medical Assessment of U.S.-Bound Refugees
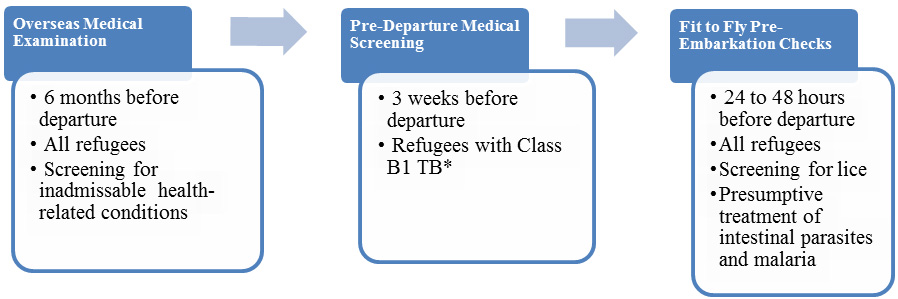
*Class B1 TB refers to TB fully treated by directly observed therapy, or abnormal chest x-ray with negative sputum smears and cultures, or extrapulmonary TB.
An overseas medical examination (CDC: Overseas Refugee Health Guidance) is mandatory for all refugees coming to the United States and must be performed according to CDC: Technical Instructions for Panel Physicians. The purpose of the overseas medical examination is to identify applicants with inadmissible health-related conditions. These examinations are performed by panel physicians who are selected by Department of State (DOS) Consular Officials. In some countries, the panel physicians are from the International Organization for Migration (IOM). CDC provides the regulatory and technical oversight and training for all panel physicians. Information collected during the refugee overseas medical examination is reported to CDC’s Electronic Disease Notification System (EDN) and is available to the state refugee health programs in the areas where the refugees are resettled.
For refugees previously diagnosed with Class B1 TB (TB fully treated using DOT, or abnormal chest X-ray with negative sputum smears and cultures, or extrapulmonary TB) a pre-departure medical screening is conducted about three weeks before departure for the United States. The screening includes a repeat physical examination, with a focus on TB signs and symptoms, chest X-ray, and sputum collection for acid fast bacilli (ADB) smear microscopy.
For all departing refugees, IOM clinicians perform two pre-embarkation checks within 48 hours of the refugee’s departure to the United States to assess their health for travel and to administer presumptive therapy for intestinal parasites (worms).
Burmese refugees departing from Thailand and Malaysia receive pre-departure treatment for soil-transmitted helminthes (Ascaris, whipworm and hookworm), according to current CDC: Overseas Refugee Health Guidance. Except when contraindicated, soil-transmitted helminths are presumptively treated with a single dose of albendazole and Strongyloides with two consecutive days of ivermectin.
Information on presumptive therapy for intestinal parasites will be noted on IOM’s Pre-departure Medical Screening form included in the packet provided for each refugee during the pre-departure process. Information on presumptive therapy for intestinal parasites given to refugees will also appear in CDC’s EDN.
Once refugees have arrived in the United States, CDC recommends that they receive a domestic medical screening within 90 days of arrival (CDC: Guidance for the U.S. Domestic Medical Examination for Newly Arriving Refugees). The purpose of these comprehensive domestic medical examinations is to identify conditions that may not have been screened for during overseas medical examinations and to serve as an introduction to the U.S. healthcare system. CDC provides guidance and recommendations to state and local refugee health partners who conduct the domestic screenings. Data from the screenings are collected by most state health departments.
Health conditions to consider in post-arrival medical screening
Communicable diseases
Malaria is prevalent in Myanmar, with the most common species being P. falciparum (which causes acute malaria) and P. vivax (which may cause acute malaria or become dormant in the liver, emerging months, or even years, later, causing clinical malaria). Refugee camps are situated in Thailand along the border with Myanmar, and there is frequent travel between the two countries. Although malaria in Thailand is unusual, this cross-border travel and the proximity to Myanmar creates an opportunity for acute clinical cases of malaria in Burmese refugees residing in these camps. There is no sustained malaria transmission in Kuala Lumpur, Malaysia. Refugees originating from Malaysia (Kuala Lumpur) are not at risk of acute malaria. However, most Burmese refugees who have resided in Myanmar have had exposure to areas of P. vivax during their lifetime and may harbor dormant infection. This infection may reactivate following immigration to the United States. At present, the presumptive antimalarial treatment program for refugee populations at high risk of malaria prior to immigration to the United States is only in effect in sub-Saharan Africa. At this time, malaria prevalence rates in Burmese refugees in Thailand are not substantial enough to warrant presumptive treatment in this population. Refugees with P. falciparum infection who are from regions of lower prevalence would be expected to show clinical signs of disease (in highly endemic areas, such as many areas of Africa, P. falciparum malaria parasitemia may be asymptomatic or sub-clinical). In addition, common medications used to treat acute malaria do not treat the dormant liver phase of P. vivax.
The clinician should be aware that clinical malaria may occur in Burmese refugees, with those originating in Thailand at highest risk. In addition, it should be noted that P. vivax relapse may occur many months, or even years, following migration. Any patient with clinical signs and symptoms of malaria should be tested for infection. The CDC provides clinical consultation support for providers seeking information on the diagnosis and management of malaria.
There are a number of intestinal parasitic infections that may be encountered in Burmese refugees. These are often parasites found commonly in populations residing in tropical areas, such as Ascaris, Trichuris, hookworm, and Giardia. This section will discuss specific infections that may be unique to, or of particular concern, in this population.
Strongyloidiasis is a parasitic nematode infection that is common in Asian refugees and is known to persist for more than 50 years in the human host. Infection is frequently asymptomatic, but may lead to morbidity and, when the infected individual is immunosuppressed, even result in death.
Unpublished data from Minnesota have found seroprevalence of Strongyloides infection among Burmese refugees originating in Thailand who arrived in the United States in 2009-2012 to be ~10% (241/2304). Another study of Karen Burmese refugees arriving in Australia from Thailand (2006-2009) found a seroprevalence of 21%, and unpublished serologic data of Burmese refugees arriving in Texas showed a rate of 40% (191/663) of the samples tested 8. Although only limited serologic data on Burmese refugees originating in Malaysia exist, of 995 serum specimens tested, 21% (198) of samples were positive. The CDC currently recommends that all U.S.-bound Burmese refugees either be presumptively treated for strongyloidiasis overseas or, if they have not been treated overseas, be tested and treated (if positive) after arrival in the United States.
The treatment of choice for Strongyloides infection is ivermectin, given once daily for two consecutive days. Currently, all resettlement eligible Burmese refugees, whether they originate in Thailand or in Malaysia, are receiving ivermectin prior to departure for the United States. Ivermectin is thought to be more than 90% effective in treating Strongyloides infection, although it may not eradicate all infections9. If a refugee has persistent symptoms, or persistent eosinophilia (> 3 months after arrival in the United States), strongyloidiasis should still be considered in the differential diagnosis. In this case, it is reasonable to perform serologic testing and/or repeat presumptive treatment, especially if the patient will be immunosuppressed or placed on corticosteroids.
For the domestic guidelines for diagnosis and management of parasites in refugees, please see the current CDC: Presumptive Treatment and Screening for Strongyloidiasis, Infections Caused by Other Soil-Transmitted Helminths, and Schistosomiasis among Newly Arrived Refugees.
Cysticercosis is an infection with the larval stage of the parasitic cestode (tapeworm) Taenia solium. Both pigs and humans may be infected by ingesting eggs or gravid proglottids. The adult tapeworm resides in the human intestine, where it occasionally may causes mild gastrointestinal symptoms. This is called taeniasis. Cysticercosis is usually caused when a human ingests eggs shed in the feces of a human tapeworm carrier (although they may also experience cysticercosis from autoinfection). Cysticercosis occurs when oncospheres hatch in the intestines and invade the intestinal wall, migrating into striated muscle, the brain, liver, or other tissues, where they develop into cysts (“cysticerci”). When cysticerci are found in the central nervous system, the infection is referred to as neurocysticercosis (NCC), which, when symptomatic, most commonly presents with seizures. Treatment of NCC is complicated, and consultation with a specialist familiar with this disorder is recommended prior to initiating treatment.
Inadvertent treatment of a person with NCC with certain antiparasitics (e.g., albendazole, praziquantel) may precipitate symptoms such as seizures. Therefore, patients with known NCC or a seizure disorder should not be treated with these medications until a formal neurologic evaluation has been performed.
Although data specific to Burmese refugees are not available, intestinal infection with the adult tapeworm (taeniasis) is typically seen on stool ova and parasite (O&P) screening in ~1-2% of all refugees following arriving in the United States. It is not possible to distinguish between T. solium and other Taenia tapeworms on stool O&P unless a proglottid is seen. While routine stool studies of asymptomatic refugees are not indicated given this low overall prevalence rate, when a family member has known infection (either intestinal or cysticercosis), screening of family members and close contacts stool and ova parasite examinations is indicated. In addition, diagnostic testing with stool O&Ps should be considered in those with gastrointestinal signs or symptoms, if they report or bring in a proglottid passed in their stool (generally about the size of a piece of rice). Use of albendazole or praziquantel should be restricted to those without a history of seizures or known NCC. Assistance with screening, diagnosis, and treatment may be obtained from CDC Division of Parasitic and Malaria Diseases (DPDM): Parasites.
Trematode (“fluke”) infections occur worldwide, but each infection has a specific geographic distribution. Human infection is largely determined by dietary or environmental exposure in endemic areas. All fluke infections may be persistent and last many years following exposure. Although the most common trematode infection is schistosomiasis, considered the only “blood-fluke”, Myanmar, areas of Thailand and Malaysia, where refugees from Burma have resided, are not endemic. However, other trematodes that may be encountered in these refugees and include: Paragonimus westermani (lung fluke), the liver flukes (Clonorchis sinensis, Fasciola hepatica, Opisthorchis viverrini) and the intestinal flukes (Fasciolopsis buski, Heterophyes heterophyes, and Metagonimus yokogawai). These trematode infections are acquired through ingestion of specific food items. Although Burmese refugees may be exposed to multiple trematode species, the most commonly encountered trematodes in this population are Paragonimus westermani and Clonorchis sinensis, which are discussed below.
Paragonimiasis
Paragonimus, also known as lung fluke, is acquired from eating raw or undercooked freshwater crab or crayfish, which is a common practice in many Burmese populations (where preparation of these crustaceans is done with vinegar, brine, or wine without cooking; therefore, failing to kill the organism). Following consumption of the metacercariae and the development of the adult worm, Paragonimus will make its way to the pulmonary system, where it induces inflammation and generates fibrous cysts containing purulent, bloody fluid and may cause an effusion. The eggs are subsequently released into the environment through expectoration, or may be swallowed and passed in the stool. Most infected individuals have no or subtle symptoms. The most common clinical presentation resembles a chronic bronchitis or tuberculosis with cough, which is frequently productive of coffee-colored or blood tinged sputum, chest pain, and/or shortness of breath. The sputum may be “peppered” with visible clumps of eggs. It commonly causes chest radiograph (CXR) abnormalities such as lobar infiltrates, coin lesions, cavities, calcified nodules, hilar enlargement, and, particularly, pleural thickening and effusions. CXR findings of “ring-shaped opacities” of contiguous cavities, often referred to as a “grapebunch,” is suggestive of this infection. Central nervous system (CNS) infection does occur and should be considered in persons with symptoms such as headaches, seizures, visual changes, or other CNS symptoms. Paragonimus may also invade the liver, spleen, intestinal wall, peritoneum, and abdominal lymph nodes.
No Paragonimus prevalence data are available in Burmese refugees, but there have been many clinical cases diagnosed in refugees following their arrival in the United States. Diagnosis can be challenging, but for patients with pulmonary signs or symptoms, sputum O&Ps examination may be helpful (note: acid fast bacilli staining for TB will destroy the eggs and sputum O&P should not be stained for acid fast bacilli). Stool O&P may be diagnostic, but has low sensitivity for detecting infection. Serum antibody testing is also available. Information about Paragonimus, including information on diagnosis and treatment, is available at CDC: Paragonimiasis. Generally, when paragonimiasis is suspected, an expert should be consulted.
Clonorchis sinensis
Clonorchis (“liver fluke”) infects the liver, gallbladder, and bile ducts. In addition to humans, the reservoir species include dogs and other fish-eating carnivores. Infection is acquired when a human ingests raw, salted, pickled, smoked, marinated, dried, partially or poorly cooked fish. Most individuals have no or minimal symptoms. The most common finding in refugees is a persistently elevated eosinophil count. Common symptoms include fever, right-upper quadrant pain, and intermittent biliary colic pain (when the worms obstruct the biliary tract). Chronic infection may result in recurrent pyogenic cholangitis, and is associated with cholangiohepatitis. Infection may be confused with gallstones and cholecystitis (tip: on ultrasound, the fluke is echogenic and appears dark, compared to a gallstone, which is generally lighter in appearance). Chronic infection with Clonorchis sinensis has been associated with biliary cancer, and the International Agency for Research on Cancer (IARC) has classified it as a Group 1 agent (carcinogenic in humans).
Risk of infection is highly dependent on diet, and the infection has been detected in Burmese refugees (the greatest number of cases in U.S. refugees historically has occurred in the Hmong)7. When suspected, the first diagnostic tests indicated are multiple stool O&Ps and ultrasound of the liver and biliary tract. Diagnosis can be challenging, since these tests are not sensitive. Serologic testing is available outside the United States. Generally, when Clonorchis infection is suspected, an expert should be consulted. Further information is available from CDC Clonorchiasis: Resources for Health Professionals.
Chlamydia and gonorrhea
The current CDC: Sexual and Reproductive Health Screening during the Domestic Medical Examination for Newly Arrived Refugees suggest routine screening for chlamydia in women < 25 years old who are sexually active, and testing any refugees with known risk factors or signs of infection for chlamydia and gonorrhea.
There are limited data available on rates of chlamydia and gonorrhea in Burmese refugees. Unpublished data screening data from Minnesota showed that of the approximately 33% of Burmese refugee arrivals who were screened from 2009-2012, only 1% (11/1007) were positive for chlamydia and 0% (0/982) were positive for gonorrhea (Table 3). All cases of chlamydia occurred in persons aged 15-44 years of age. No data have been published or identified regarding rates of chlamydia or gonorrhea in Burmese refugees originating in Malaysia. Prevalence in Burmese refugees arriving from Malaysia may differ from those originating from Thailand because, for example, Malaysian refugees largely live in urban centers (while those from Thailand residing in refugee camps, often in rural areas). However, given the low rates reported in those from Thailand and the overall low rates in refugees, the current CDC guidelines are felt to be sufficient for these populations (screening for chlamydia in women < 25 years old who are sexually active, or testing refugees for chlamydia and gonorrhea if there are known risk factors or signs of infection [e.g., discharge, elevated white blood count, or leukocyte esterase-positive urine sample]).
Table 3. Chlamydia and Gonorrhea Results Among Burmese Primary Refugee Arrivals to Minnesota, 2009-2012
| Age at U.S. Arrival (years) | No. Screened* | Screened for Chlamydia No. (%) | Positive Chlamydia Result No. (%) | Negative Chlamydia Result No. (%) |
|---|---|---|---|---|
| 0-5 | 440 | 5 (1%) | 0 (0%) | 5 (100%) |
| 5-14 | 763 | 33 (4%) | 0 (0%) | 33 (100%) |
| 15-24 | 748 | 412 (55%) | 6 (1%) | 406 (99%) |
| 25-44 | 749 | 376 (50%) | 5 (1%) | 371 (99%) |
| 45-64 | 296 | 154 (52%) | 0 (0%) | 154 (100%) |
| 65+ | 54 | 27 (50%) | 0 (0%) | 27 (100%) |
| Total | 3,050 | 1,007 (33%) | 11 (1%) | 996 (99%) |
| Age at U.S. Arrival (years) | No. Screened* | Screened for Gonorrhea No. (%) | Positive Gonorrhea Result No. (%) | Negative Gonorrhea Result No. (%) |
|---|---|---|---|---|
| 0-5 | 440 | 4 (1%) | 0 (0%) | 4 (100%) |
| 5-14 | 763 | 33 (4%) | 0 (0%) | 33 (100%) |
| 15-24 | 748 | 392 (52%) | 0 (0%) | 392 (100%) |
| 25-44 | 749 | 373 (50%) | 0 (0%) | 373 (100%) |
| 45-64 | 296 | 154 (52%) | 0 (0%) | 154 (100%) |
| 65+ | 54 | 26 (50%) | 0 (0%) | 26 (100%) |
| Total | 3,050 | 982 (32%) | 0 (0%) | 982 (100%) |
*Received a post-arrival refugee health assessment, usually initiated within 90 days of U.S. arrival.
Human Immunodeficiency Virus
Refugees resettling to the United States do not receive routine pre-departure/overseas screening for HIV infection. It is currently recommended that all refugees be screened for HIV following arrival in the United States (CDC: Screening for HIV Infection During the Refugee Domestic Medical Examination). Unpublished data from Texas (2009-2012) showed that 1.7% (84/4831) of Burmese refugees originating from Malaysia and 0.3% (14/4146) of Burmese refugees originating from Thailand had HIV infection. Similar data from Minnesota (2009-2012) reported a low prevalence among Burmese refugees arriving in Minnesota from Thailand (2/2505). Given that early identification and treatment of infection reduces morbidity and mortality and decreases transmission, it remains imperative that refugees receive post-arrival HIV screening.
Syphilis
All refugees > 15 years of age are required to have syphilis testing prior to departure for the United States. Unpublished data from Texas showed that ~0.5% of Burmese refugees (n=7458) had a positive screening test for syphilis. The current CDC: Sexual and Reproductive Health Screening during the Domestic Medical Examination for Newly Arrived Refugees note that repeat testing is not necessary when overseas documentation is available. When documentation is not available, refugees > 15 years of age should receive testing during the domestic medical evaluation. In children younger than 15 years or age, testing should be performed on those who are at risk (i.e., mother tests positive for syphilis). Guidance regarding syphilis testing and treatment is available in the CDC Sexually Transmitted Diseases Treatment Guidelines, 2010.
Hepatitis B and C
Persons with chronic hepatitis B virus (HBV) infection are at risk for developing chronic liver disease, including cirrhosis and hepatocellular carcinoma, as well as extrahepatic manifestations such as glomerulonephritis. Burmese refugees originating in Thailand have been documented to have a chronic HBV infection prevalence of 8-10% (6,569 refugees screened from 2009-2012 in Minnesota and Texas). Prevalence in Karen Burmese refugees originating from Thailand and arriving in Australia was similar at 9.7% (of 1136 new arrivals)8. Data from Burmese refugees originating in Malaysia are more limited, but among 5,102 refugees screened in Texas from 2009-2012, there was a 6% rate of chronic HBV infection. It is currently recommended that all refugees from countries with rates > 2% be screened for chronic HBV infection (CDC Yellow Book 2024: Hepatitis B), which include all groups of Burmese refugees (CDC: Screening for Viral Hepatitis During the Domestic Medical Examination of Newly Arrived Refugees).
Chronic infection with hepatitis C virus (HCV) may also lead to cirrhosis and hepatocellular carcinoma. The current recommendations for screening for HCV infection in the United States include routine screening of those born between 1945 and 1965, and screening of persons with known risk factors for HCV infection (such as patients with history of injection drug use, HIV-positive patients, patients who received blood products prior to migration, children of parents with known hepatitis C). Data on HCV infection rates in refugees are limited, and, currently, the CDC domestic screening guidelines recommend that refugees be screened according to existing CDC guidelines for the United States population. In Minnesota from 2009-2012, 1,746 (56%) Burmese refugees arriving from Thailand were screened for HCV infection (n=3050). Of these, 54 (3%) screened positive for HCV infection, with 34 found to have confirmed infection by viral load (for an overall rate of 2.2%). The highest prevalence of HCV infection was among those aged 45-64 years (Table 4). Screening data from Texas over the same time period identified a 2.2% (79/3557) seropositive rate in Burmese refugees originating in Thailand and a 2.8% (113/4098) seropositive rate in Burmese refugees originating in Malaysia (confirmatory testing not available). Since Minnesota and Texas do not routinely screen all refugees and instead focus on those in higher-risk groups, these rates may be inaccurately elevated since clinicians are more likely to test those at increased risk for infection. Data from Karen Burmese refugees arriving in Australia showed a similar HCV infection rate of 1.9% (n=1136)8. A majority of cases occurred among those aged 45-64 years. These data indicate that routine screening should be done in arriving refugees born between 1945 and 1965, as well as those with known risk factors.
Table 4. Hepatitis C Screening Among Burmese Primary Refugee Arrivals to Minnesota, 2009-2012
| Age at U.S. Arrival (years) | No. Screened* | Screened for Hepatitis C ** No. (%) | Positive Hepatitis C Result No. (%) | Negative Hepatitis C Result*** No. (%) | Indeterminate Hepatitis C Result No. (%) |
|---|---|---|---|---|---|
| 0-5 | 440 | 237 (1%) | 0 (0%) | 237 (100%) | 0 (0%) |
| 5-14 | 763 | 410 (4%) | 0 (0%) | 410 (100%) | 0 (0%) |
| 15-24 | 748 | 448 (55%) | 6 (1%) | 440 (98%) | 2 (<1%) |
| 25-44 | 749 | 439 (50%) | 21 (5%) | 417 (95%) | 1 (<1%) |
| 45-64 | 296 | 180 (52%) | 25 (14%) | 153 (85%) | 2 (1%) |
| 65+ | 54 | 32 (50%) | 2 (6%) | 30 (94%) | 0 (0%) |
| Total | 3,050 | 1,746(32%) | 54 (3%)**** | 1,689 (97%) | 5 (<1%) |
*Received a post-arrival refugee health assessment, usually initiated within 90 days of U.S. arrival
**Screened using hepatitis C antibody (anti-HCV) test
*** Recorded as negative if initial anti-HCV result positive and confirmatory result negative
****34 (63%) with a known positive confirmatory test result and 6 (11%) with an indeterminate confirmatory test result
Non-communicable diseases and injuries
Non-communicable diseases are understudied and poorly documented among the Burmese. Chronic hepatitis B infection is present in approximately 15% of the Burmese population, and oral health problems are common [5]. Domestic screening of resettled refugees from Myanmar in 2009, showed that 13% of children had an elevated blood lead level (EBLL), compared with 1% of all children in the United States [10]. Risk factors for EBLL among refugees resettled to the United States include: living in older homes with lead hazards; cultural practices involving traditional medicines; compromised nutritional status; and, lack of education about lead poisoning [11].
Refugees from Myanmar are susceptible to acute and severe undernutrition, presenting as marasmus and kwashiorkor, as well as cachexia, chronic undernutrition, and micronutrient deficiencies [5]. High rates of acute and chronic malnutrition are not well-documented, but are likely true because over 40% of Burmese children younger than age 5 in western Myanmar are stunted and one-third are underweight [12]. In 2003, 72% of children from Myanmar had anemia, compared to 49% for children younger than age 5 in the rest of Southeast Asia [13].
Burmese refugees being resettled to the United States are likely to have some level of mental health problems. Within Myanmar, many are subjected to torture by the Burmese Army, including: forced labor; stress positions; beatings; burning; sexual assault, rape; electric shock; sleep deprivation; and, solitary confinement [2]. Human trafficking occurs within Myanmar and from Myanmar to East and Southeast Asia [2]. Alcoholism also may be common among resettled Burmese refugees, especially men [14].
- Central Intelligence Agency. Burma. World Factbook; Available from: https://www.cia.gov/library/publications/the-world-factbook/geos/bm.html.
- Gulf Coast Jewish Family & Community Services, Country Conditions Report: Burma. 2015.
- Bower, B.L., et al., Reaching out to Burmese Refugees, in TB & Cultural Competency, Notes from the Field. 2008, Northeastern Regional Training and Medical Consultation Consortium.
- Barron, S., et al., Refugees from Burma: Their Backgrounds and Refugee Experiences. 2007, Center for Applied Linguistics: Washington, DC.
- U.S. Department of Health and Human Services. Background on Potential Health Issues for Burmese Refugees. 2010 [cited 2011 June 24]; Available from: www.globalhealth.gov.
- The Border Consortium, The Border Consortium Programme Report. 2014.
- Stauffer, W.M., J.S. Sellman, and P.F. Walker, Biliary liver flukes (Opisthorchiasis and Clonorchiasis) in immigrants in the United States: often subtle and diagnosed years after arrival. J Travel Med, 2004. 11(3): p. 157-9. Added.
- Paxton, G.A., et al., Post-arrival health screening in Karen refugees in Australia. PLoS One, 2012. 7(5): p. e38194. Added.
- Gann, P.H., F.A. Neva, and A.A. Gam, A randomized trial of single- and two-dose ivermectin versus thiabendazole for treatment of strongyloidiasis. J Infect Dis, 1994. 169(5): p. 1076-9. Added.
- Mitchell, T., et al., Elevated Blood Lead Levels among Children in Refugee Camps Mae La, Umpiem, and Nupo. 2009, Centers for Disease Control and Prevention Refugee Camps, Tak Province, Thailand.
- New York State Department of Health, Working with Refugees from Myanmar to Prevent Childhood Lead Poisoning. 2010.
- Sollom, R., et al., Health and human rights in Chin State, Western Burma: a population-based assessment using multistaged household cluster sampling. PLoS Med, 2011. 8(2): p. e1001007. Added.
- Stover, E., et al., The Gathering Storm: Infectious Diseases and Human Rights in Burma. 2007, Human Rights Center, University of California-Berkeley, and Center for Public Health and Human Rights, Johns Hopkins Bloomberg School of Public Health.
- International Rescue Committee, The Health of Refugees from Burma. 2009.
