Contact Info
About Mpox
On this page:
Symptoms
How it spreads
Prevention
Vaccine
Testing
Treatment
Materials
More about mpox
Mpox, previously known as monkeypox, is an uncommon disease caused by the mpox virus. Mpox virus is in the same family of viruses as the variola virus that causes smallpox.
Prior to 2022, mpox was spread mostly through contact with certain animals. During the global mpox outbreak that began in May of 2022 we saw mpox mostly spread through close physical contact between people. Some populations were affected more than others, including gay, bisexual, and other men who have sex with men who had recent contact with a new partner or partners.
Symptoms
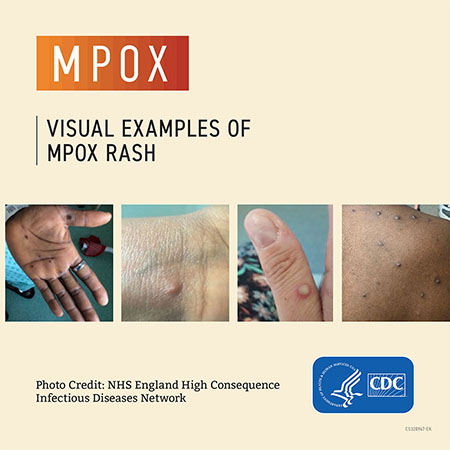
Mpox symptoms often include a rash that can look like pimples or blisters. The rash can appear on the face, inside the mouth, and on other parts of the body, like the hands, feet, chest, genitals, or anus. Symptoms develop approximately 12 days after a person has been exposed but may be as early as five days and as late as 21 days.
Other symptoms of mpox can include:
- Fever or chills
- Swollen lymph nodes
- Headache
- Fatigue
- Body aches
Some people do not report having symptoms before the onset of rash. In most cases the rash begins as a flat rash, then progresses to raised bumps which become filled with fluid (poxes). Eventually the rash crusts over and scabs develop. Some people may have only one sore, bump, or blister. This may look different from pictures you see online.
A person is infectious from symptom onset until scabs fall off and a fresh layer of healthy skin has formed. The illness can last for around two to four weeks.
How it spreads
Mpox is spread through direct and indirect contact with the virus.
- Human-to-human transmission:
- Prolonged direct contact with body fluids or skin lesions (i.e., skin to skin contact) is the most common mode of human-to-human transmission.
- Clothing, bedding, and other objects:
- Transmission can occur from contact with contaminated clothing/bedding/towels or other objects used by a person with mpox.
- Animal-to-human transmission:
- Animal-to-human transmission may occur through a bite or scratch, preparation of wild game, and direct or indirect contact with body fluids or rash material (not a mode of transmission in the U.S.).
Prevention
Take the following steps to prevent or decrease your risk for getting mpox:
- Avoid close, prolonged skin-to-skin contact, and sex (oral, anal, vaginal) with people whose infection status is unknown or with a history of recent travel to areas that are part of a current mpox outbreak.
- Avoid close contact with people who have a rash that looks like mpox.
- Do not handle or share the bedding, towels, or clothing used by a person with mpox.
- Wash your hands often with soap and water or use an alcohol-based hand sanitizer.
Visit Lower Your Risk for Mpox for more information about steps you can take to reduce your risks for getting mpox.
Vaccine
Vaccination is the best way to protect against mpox infection and is recommended for those who are at risk or have been exposed to a person who has mpox. The mpox vaccine is given as a two-dose series separated by 28 days (four weeks).
People who are at risk of mpox disease:
- You had known or suspected exposure to someone with mpox.
- You had a sex partner in the past two weeks who was diagnosed with mpox.
- You are a gay, bisexual, or other man who has sex with men or a transgender, nonbinary, or gender-diverse person who in the past six months has had any of the following:
- A new diagnosis of one or more sexually transmitted diseases (e.g., chlamydia, gonorrhea, or syphilis).
- More than one sex partner.
- You have had any of the following in the past six months:
- Sex at a commercial sex venue (like a sex club or bathhouse).
- Sex related to a large commercial event or in a geographic area (city or county for example) where mpox virus transmission is occurring.
- You have a sex partner with any of the above risks.
- You anticipate experiencing any of the above scenarios.
- You are at risk for occupational exposure to orthopoxviruses (e.g., certain people who work in a laboratory or a health care facility)
For more information, refer to CDC: Mpox Vaccine Recommendations. People exposed to a person with confirmed or probable mpox CDC recommends getting vaccinated within four days from the first day you were exposed to help prevent disease. If given between four and 14 days after exposure, vaccination may reduce the symptoms but may not prevent infection. Talk to your health care provider if it has been more than 14 days after exposure. Refer to CDC: If You’re a Close Contact for more information.
If you are at risk and would like to get vaccinated, start by contacting your primary health care provider. If you do not have a provider or your provider does not have vaccine, visit CDC: Mpox Vaccination Basics to search the CDC: Find Mpox Vaccines tool to find a vaccine provider or clinic that has reported they have vaccine available.
Make sure you are up to date with your mpox vaccination. It is possible to get mpox even after getting vaccinated, but getting both doses of the vaccine makes getting and spreading mpox less likely. The vaccine may also help make symptoms less severe and easier to manage, and may help protect you against severe infection, hospitalization, and death. For more information visit CDC: Mpox after Vaccination.
Testing
If you have a new rash, sore, pimple-like bump, or blister, get tested. Only people who have a rash can get tested for mpox. You may be asked questions about sexual activity/behaviors by your provider to determine if testing for mpox is necessary. The mpox rash may look like other sexually transmitted infections (STIs) such as syphilis or herpes so your provider may consider additional STI testing.
Consult with a health care provider. If you do not have a health care provider, consider one of the following free or low-cost testing sites:
- Red Door Clinic/ Hennepin County Public Health
612-543-5555
525 Portland Avenue South, Minneapolis MN - Clinic 555 / Ramsey County Public Health
651-266-1352
555 Cedar Street, St. Paul MN - Aliveness Project
612-824-5433
3803 Nicollet Avenue, Minneapolis, MN 55409 - Health Centers
Information about Federally Qualified Health Centers (FQHCs), including a link to search for a health center.
Treatment
There is no specific treatment for mpox, although treatment with an antiviral, Tecovirimat (TPOXX), may be recommended for people who are more likely to get severely ill, like patients with weakened immune systems. In certain situations, people who have been exposed to someone with mpox may benefit from receiving a mpox vaccine.
Materials
 | Protect Yourself From Mpox(PDF) Protéjase De La Viruela Símica O Del Mono (PDF) |
 | Mpox (one palm card) (PDF) Mpox (four palm cards) (PDF) |
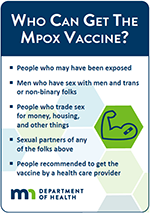 | Who Can Get the Mpox Vaccine? (one palm card) (PDF) Double-sided, print size is 4.25 x 5.5 inches, card can be cut to 3.25 x 4.625 inches Who Can Get the Mpox Vaccine? (four palm cards) (PDF) Four double-sided cards on letter size paper |
MCN: New Low-Literacy Mpox Resource, in English & Spanish
Migrant Clinicians Network simple resource in English and Spanish that helps explain the spread of mpox, as well as identifying symptoms and isolation strategies for those who may be infected.
About Mpox ASL Video