Annual Summary of Disease Activity:
Disease Control Newsletter (DCN)
Related Topics
Contact Info
Campylobacteriosis, 2017
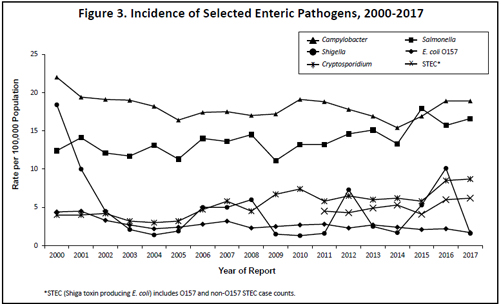
There were 1,049 culture-confirmed Campylobacter cases reported in 2017 (18.9 per 100,000 population). This is similar to the 1,042 cases reported in 2016, but a 14% increase from the annual median of 917 cases reported from 2007 to 2016 (range, 834 to 1,042). In 2017, 44% of cases occurred in people who resided in the metropolitan area. Of the 981 Campylobacter isolates confirmed and identified to species by MDH, 84% were C. jejuni and 9% were C. coli.
The median age of cases was 39 years (range, 4 months to 91 years). Forty-one percent were between 20 and 49 years of age, and 10% were ≤5 years of age. Fifty-five percent were male. Fifteen percent were hospitalized; the median length of hospitalization was 2 days. Forty-eight percent of infections occurred during June through September. Of the 959 cases for whom data were available, 167 (17%) reported travel outside the United States during the week prior to illness onset. The most common travel destinations were Europe (n=41), Asia (n=40), Central or South America or the Caribbean (n=35), Mexico (n=30), Africa (n=12), and the Middle East (n=7).
One foodborne outbreak was identified in 2017. Two culture-confirmed C. jejuni infections were associated with an event at a restaurant. The vehicle of transmission was suspected to be raw oysters.
A primary feature of public health importance among Campylobacter cases was the continued presence of Campylobacter isolates resistant to fluoroquinolone antibiotics (e.g., ciprofloxacin), which are commonly used to treat campylobacteriosis. In 2017, the overall proportion of quinolone resistance among Campylobacter isolates tested was 28%. However, 80% of Campylobacter isolates from patients with a history of foreign travel during the week prior to illness onset, regardless of destination, were resistant to fluoroquinolones. Eighteen percent of Campylobacter isolates from patients who acquired the infection domestically were resistant to fluoroquinolones.
In 2009, a culture-independent test (CIDT) became commercially available for the qualitative detection of Campylobacter antigens in stool. In 2017, 420 patients were positive for Campylobacter by an antigen detection CIDT conducted in a clinical laboratory. However, only 133 (32%) of the specimens were subsequently culture-confirmed. Beginning In 2015, some clinical laboratories in Minnesota began testing stool specimens with PCR-based gastrointestinal pathogen panels, another type of CIDT. In 2017, 791 patients were positive for Campylobacter by a PCR gastrointestinal panel; 575 (73%) of these specimens were culture-confirmed. Only culture-confirmed cases met the surveillance case definition for inclusion in MDH case count totals.
- For up to date information see>> Campylobacteriosis (Campylobacter)
- Full issue>> Annual Summary of Communicable Diseases Reported to the Minnesota Department of Health, 2017