
Health Care Homes Sustainability Roadmap
Finance
"The fragility of primary care remains rooted in the lack of tangible progress on financing — specifically, how and how much primary care practices are paid. Yet, policy shifts at both federal and state levels have the potential to drive significant change in the years ahead."
Reimbursement, incentives, alternative payment arrangements, value-based contracting, and optimized revenue streams are critical to financial stability. Certified Health Care Homes (HCH) in Minnesota can obtain reimbursement for care coordination and leverage participation in programs such as the Centers for Medicare & Medicaid Services (CMS) Quality Payment Program (QPP). HCH certification also prepares organizations for success in value-based payment arrangements.
Strategies
Implementing the following strategies can help Health Care Homes maximize financial sustainability while supporting high-quality, team-based primary care. Leveraging value-based payment models, optimizing care coordination reimbursement, pursuing advanced certification levels, and exploring grant opportunities, can create more stable revenue streams and increased efficiency.
- Leverage Physician Maintenance of Certification (MOC) Credits
Receive credit for practicing in a certified Health Care Home:- American Board of Family Medicine: refer to the Recognitions/Certifications section of the Performance Improvement At-A-Glance (PDF)
- Patient-Centered Medical Home (PCMH) | The American Board of Pediatrics.
- Pursue Alternative Payments and Value-Based Arrangements
Engage with state and national programs, accountable care organizations (ACOs), and contracts recognizing the value of high-quality, team-based primary care.
- Participate in Integrated Health Partnerships
HCH certification serves as a gateway to participation in IHP, Minnesota DHS’s Medicaid ACO program. Learn more: Integrated Health Partnerships (IHP) - DHS.
- Optimize Reimbursement for Care Coordination Services
Explore billing through Minnesota Health Care Programs (MHCP) codes, per-member-per-month payments, and other alternative payment arrangements. Resources: - Participate in CMS MIPS Incentives
HCHs participating in the Merit-Based Incentive Payment System (MIPS) may qualify for additional benefits: - Pursue Advanced Certification Levels
Progressing to HCH Level 2 or Level 3 demonstrates increased capacity to address social determinants of health and health equity, opening potential new reimbursement avenues.
- Evaluate Workflows for Efficiency
Identify opportunities to improve productivity and reduce administrative burdens, creating incremental financial benefits.
- Seek Grants & Funding
Foundations, health plans, and other entities can provide funding for initiatives that advance health equity, address community needs, or improve patient outcomes.
Resources
The resources listed provide evidence-based guidance, practical tools, and policy context to support financial decision-making. They offer insights to enable certified Health Care Homes to implement sustainable financing approaches and align financial strategies with broader goals of improving health outcomes and advancing health equity.
- Implementing High-Quality Primary Care: A Policy Menu for States | National Academy for State Health Policy (NASHP)
- Office of Rural Health and Primary Care (ORHPC) Grants and Funding | Minnesota Department of Health (MDH)
- The Health of US Primary Care: 2025 Scorecard Report - The Cost of Neglect | Milbank Memorial Fund
- Primary Care: The MVP of MSSP (2024 Evidence Report) | Primary Care Collaborative (PCC)
- Administrative Burden in Primary Care: Causes and Potential Solutions | The Commonwealth Fund
- How Medicare’s 2026 Payment Rule Supports a Healthier America (PDF) | Primary Care Collaborative (PCC)
- Addressing Upstream Drivers of Health through Traditional Medicare | Partnership to Align Social Care
- Some good news for primary care: the 2026 Medicare physician fee schedule | American Academy of Family Physicians (AAFP)
- IMPROVING THE COLLECTION OF Social Determinants of Health (SDOH) Data with ICD-10-CM Z Codes (PDF) | Centers for Medicare & Medicaid Services (CMS)
- Community Health Worker Resources for Employers | Minnesota Department of Health (MDH)
- Understanding Billing for CHW Services in Minnesota - Medicare and Medicaid (YouTube video) | Minnesota Department of Health (MDH)
- Part II: Understanding Billing for CHW Services in MN 2024 (PDF) | Minnesota Department of Health (MDH)
Stories
The Health Care Homes (HCH) Sustainability Workgroup and leadership of the State Employee Group Insurance Program (SEGIP) began a collaborative project to educate SEGIP members about the benefits of HCH certification in 2019. The HCH Sustainability Workgroup’s primary objectives are to improve the health of all Minnesotans by ensuring the sustainability of certified HCH clinics and promoting population health and health equity. These goals complement SEGIP’s mission, which is to help members achieve and maintain health in every aspect of their lives by providing high-quality and cost-effective insurance and benefits.
SEGIP administers the MN Advantage Health Plan, the medical insurance program offered to state employees. It encourages members to choose cost-efficient, high-quality clinics. The Advantage Plan covers more than 130,000 members, including employees of state agencies and quasi-state units, their dependents, pre-65 retirees, and other separated employees. Members choose a primary care clinic that manages their care, and each clinic is assigned a cost level between one and four, with one being the most cost-efficient and four the least. Members are encouraged to select lower cost level clinics through reduced cost-sharing.
To help members choose the clinic that best meets their needs, SEGIP maintains a comprehensive online clinic directory that provides information on clinic location, cost level, quality, and HCH certification status. SEGIP incorporated HCH status prominently on the clinic directory starting with Open Enrollment 2022. This shows if a clinic is HCH certified, provides an informational pop-up that explains what HCH certification means for their care, and links to the HCH website for more information.
While analyzing 2022 enrollment results, SEGIP found that HCH certification was widespread in clinic networks, and the majority of members chose to receive care at a HCH certified clinic. In addition, those members enrolled at HCH certified clinics had lower average cost levels.
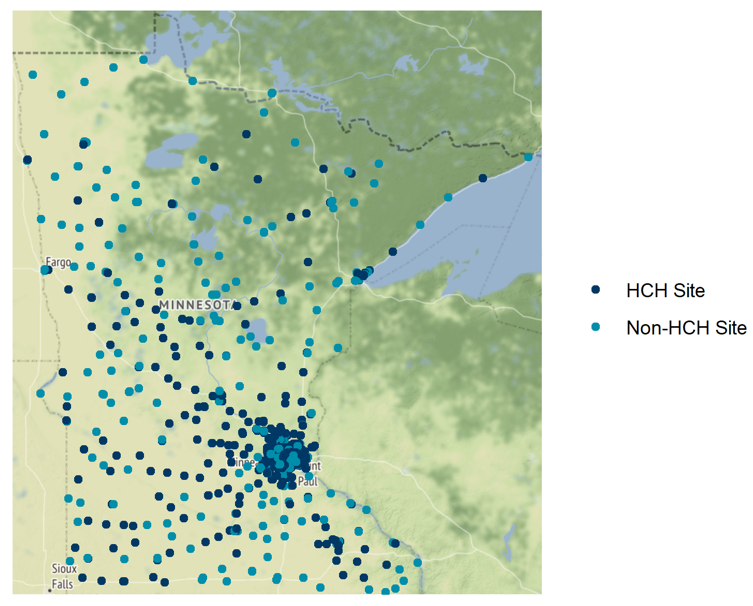
Nearly 55% of SEGIP primary care clinics in Minnesota had HCH status in 2022.
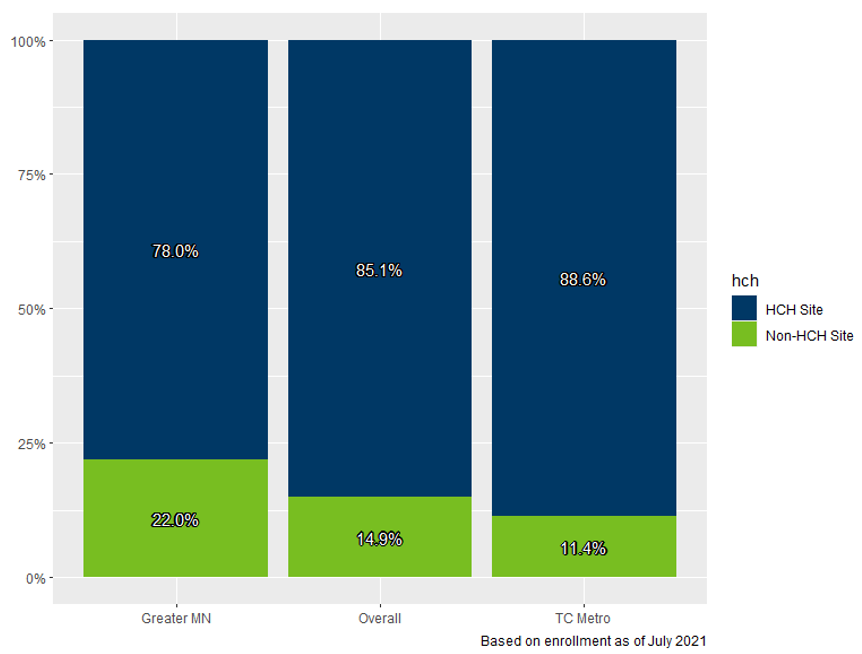
About 85% of SEGIP members in Minnesota chose an HCH as their primary care clinic for 2022.
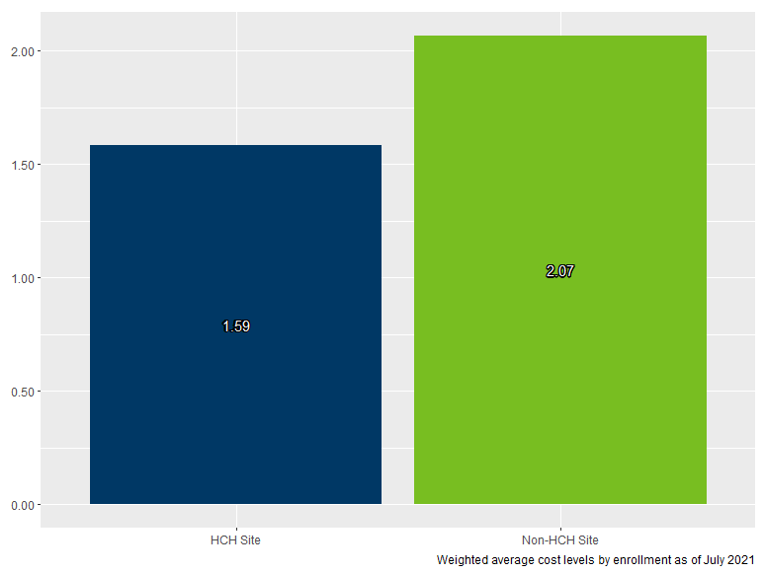
Members enrolled at HCH clinics had lower average cost levels for 2022.
“Adding Health Care Homes certification to our clinic directory has been a great way to show our members when a clinic emphasizes effective care coordination,” said Zach Holmquist, a Senior Health Care Analyst at SEGIP.
To further this collaboration, HCH and SEGIP will continue to look at new ways to improve awareness and promote the benefits of the HCH model of care.
