Public Health and Health Care Emergency Preparedness in Minnesota
Creating and sustaining public health and health care emergency preparedness, response, and recovery systems
Working together
Minnesota has invested since 1872 in maintaining healthy individuals, families, and communities. This tradition was strengthened in 1976 with the Community Health Services Act, which consolidated public health services. In recent years, there has been a new emphasis on response and recovery planning for terrorism and natural disasters among state, local, tribal, and health care partners:
- Minnesota Department of Health: Emergency Preparedness and Response; Public Health Laboratory; Mortuary Science; Environmental Health; Infectious. Disease; Epidemiology; Prevention and Control; the Communications Office; and others
- Community health boards (county and city health departments) and tribal health departments.
- Hospitals and health care facilities, through eight regional coalitions.
- State and local partners: emergency management; law enforcement; education; emergency medical services; private businesses; voluntary agencies; and others.
All emergencies are local
A key role of local health departments and health care partners in planning and response is to consider the impacts on people in a community when public health, health care, and behavioral health systems are compromised or unavailable during and after a disaster.
- Through federal funding since 2002, local, tribal and state officials have planned, trained, and practiced emergency response and recovery activities in conjunction with health care and other partners.
- With systems, structures, and wisdom growing every year, public health and health care has assisted with disaster responses throughout the state. Challenges lie ahead as federal funding dwindles. We are focusing our efforts on:
The sustainability of our systems and programs
- The continuous expansion and maintenance of partnerships and coalitions.
- Resilience and flexibility to meet all kinds of emergencies.
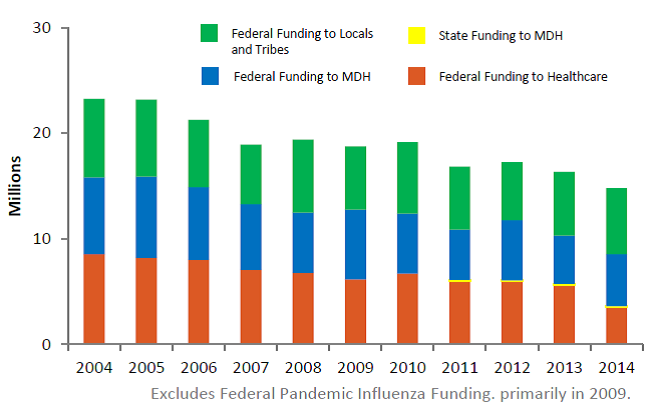
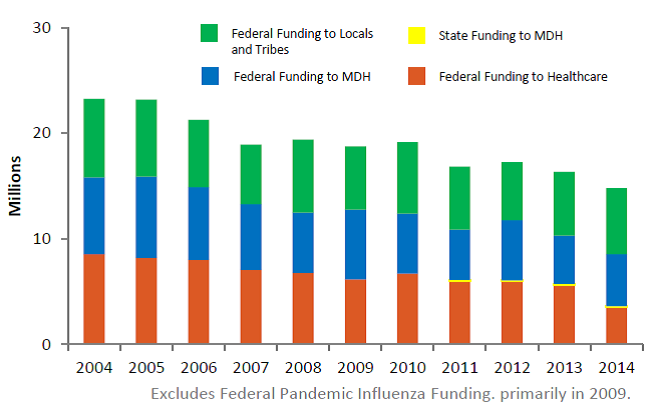
Health preparedness funding
| Year | To Hospitals | State | To Locals | MDH funding |
| 2004 | 8,542,551 | 0 | 7,248,086 | 7,453,914 |
| 2005 | 8,173,336 | 0 | 7,696,539 | 7,306,461 |
| 2006 | 7,983,328 | 0 | 6,900,400 | 6,369,600 |
| 2007 | 7,050,445 | 0 | 6,212,544 | 5,643,456 |
| 2008 | 6,761,826 | 0 | 5,715,232 | 6,901,174 |
| 2009 | 6,149,904 | 0 | 6,603,320 | 5,998,436 |
| 2010 | 6,698,777 | 0 | 5,664,216 | 6,757,310 |
| 2011 | 5,990,088 | 97,000 | 4,754,871 | 5,978,471 |
| 2012 | 5,961,891 | 100,000 | 5,693,094 | 5,491,766 |
| 2013 | 5,625,009 | 96,000 | 4,552,660 | 6,034,921 |
| 2014 | 3,526,348 | 96,000 | 4,910,827 | 6,250,144 |
Table and graphical format.
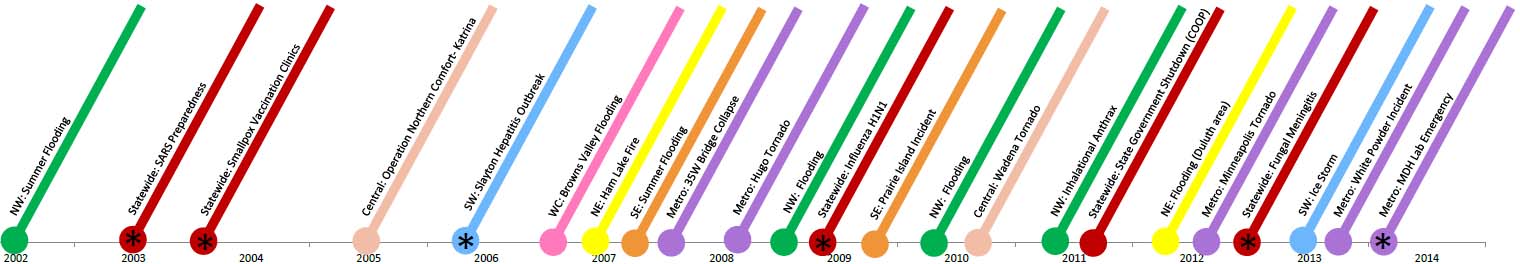
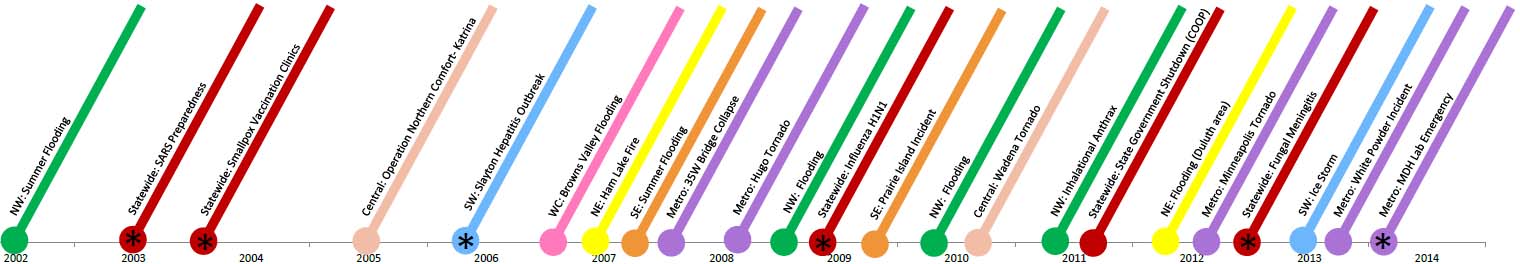
Timeline of events: 2002-2014
| 2002 | NW | Summer Flooding |
| 2003 | Statewide | SARS Preparedness |
| 2003 | Statewide | Smallpox Vaccination |
| 2005 | Central | Operation Northern Comfort - Katrina |
| 2005 | SW | Slayton Hepatitis A Outbreak |
| 2006 | WC | Browns Valley Flooding |
| 2007 | NE | Ham Lake Fire |
| 2007 | SE | Summer flooding |
| 2007 | Metro | 35W Bridge Collapse |
| 2008 | Metro | Hugo Tornado |
| 2008 | NW | Flooding |
| 2009 | Statewide | Influenza H1N1 |
| 2009 | SE | Prairie Island Incident |
| 2009 | NW | Flooding |
| 2010 | Central | Wadena Tornado |
| 2011 | NW | Inhalational Anthrax |
| 2011 | Statewide | Government Shutdown COOP |
| 2011 | NE | Flooding in Duluth area |
| 2012 | Metro | Minneapolis Tornado |
| 2012 | Statewide | Fungal Meningitis |
| 2013 | SW | Ice Storm |
| 2013 | Metro | White Powder Incident |
| 2014 | Metro | MDH Lab Emergency |
Programs
Disease surveillance: From flu to smallpox, the MDH Infectious Disease Division (IDEPC) monitors the occurrence of infectious diseases, develops strategies to prevent and control disease, and works to put those strategies into action.
Behavioral health: A range of mental health and chemical abuse (behavioral health) problems may surface at any stage in response or recovery among the public and the professionals who respond to an incident. Addressing these concerns improves the emergency response and the health of the whole community.
Health Alert Network: Alerts about developing situations or disease outbreaks are sent to local and tribal health departments who distribute them to hospitals, clinics, and others via email, phone, and fax.
Volunteer systems: In early 2004, MDH developed a registry for health professionals interested in volunteering during a public health emergency. As of the fall of 2013, 10,000 skilled and trained individuals were enrolled in the online registry.
Continuity of operations (COOP): If MDH’s own facilities, staff, or technology are compromised by a storm, power outage, or an act of sabotage, the public still counts on the agency to perform its critical functions. MDH has been developing COOP plans to be ready for any contingency.
Hospital tracking: The Minnesota System for Tracking Resources, Alerts and Communication (MNTrac) provides tracking for:
- Hospital diversion status
- Patient status
- Hospital bed availability
- Pharmaceuticals and resources MNTrac also features emergency alert and advisory notifications and online conferencing during emergencies.
Health coalitions: Health coalitions are a collaborative network of health care organizations and their respective public and private sector response partners. They facilitate resource sharing/coordination, information sharing, and coordination of incident response actions among member organizations.
Fatality management: Federal funding enabled MDH to purchase a Disaster Portable Morgue Unit and to help fund staffing for a Disaster Mortuary Emergency Response Team that will be available to help in local emergencies.
Hotlines, websites, news releases, and nurse triage lines: MDH can quickly distribute information for the public and the medical community via news releases, hotlines, and interactive websites. During the H1N1 flu pandemic, the MN FluLine received more than 27,000 calls in six months, decreasing the burden on physicians and hospitals.
Exercises and training: Statewide, regional, and local exercises are conducted regularly and systematically so all aspects of emergency planning can be tested and refined.
Medicine and medical supplies: A natural disaster or a terrorism incident could rapidly strain or deplete medical and pharmaceutical supplies. To address this, CDC developed a resource called the Strategic National Stockpile Program. It can reach any location in the United States within 12 hours of a request. Some state and local stockpiles are also in place.
Local and tribal health departments have developed and tested detailed plans to dispense medication very quickly to every Minnesotan. These mass dispensing plans rely on partners, volunteers, and the media to aid in providing medicine to the public.
Laboratory testing: The Public Health Laboratory (PHL) collaborates with a variety of program partners to detect, investigate, prevent, and control public health threats. These threats include rare or unusual infectious diseases, such as "invasive" bacterial infections; outbreaks of illness from consuming contaminated food or water; terrorism events; chemical hazards; and environmental emergencies.
Mobile medical teams: Minnesota has two mobile medical teams (MMTs), groups of volunteer medical and support professionals who have received training and practice in providing acute medical care in a mobile field environment. The MMTs can deploy either with the equipment needed to establish a range of clinical services or without equipment to support staffing needs in existing care facilities.
When resources become scarce: Patient care strategies for scarce resource situations is a standardized framework to assist Minnesota hospitals, clinics, or primary care settings in determining how to extend resources when the need for equipment and supplies exceeds availability during a health emergency.
Core strategies were developed to use during a scarce resource situation or in anticipation of one for oxygen; staffing; nutritional support; medication administration; hemodynamic support and IV fluids; mechanical ventilation; and blood products. In addition, resource reference cards designed to provide incident-specific tactics and planning information were developed for renal replacement therapy, burn therapy, pediatrics and palliative care.
Ready to respond: When a public health emergency occurs, MDH has four teams of staff trained and ready to respond. These teams maintain their readiness by conducting emergency simulation exercises several times a year.
To assist with response, MDH also has a department operations center that serves as the command center to coordinate information and activities during a response.
If communication systems are compromised, MDH has back-up cellular and satellite phones plus 800 MHz radios that are part of the statewide ARMER system. These tactical communication assets are stored at MDH and each of the seven district offices.