Annual Summary of Disease Activity
- Annual Summary Home
- Foodborne & Enteric Diseases
- Hepatitis
- Hospital-Associated Infections
- Invasive Bacterial Infections
- Sexually Transmitted Infections & HIV
- Tuberculosis
- Unexplained Deaths & Critical Illnesses
- Vaccine-Preventable Diseases
- Vectorborne Diseases
- Viral Respiratory Diseases
- Waterborne Diseases
- Zoonotic & Fungal Diseases
Related Topics
Annual Summary of Disease Activity
- Annual Summary Home
- Foodborne & Enteric Diseases
- Hepatitis
- Hospital-Associated Infections
- Invasive Bacterial Infections
- Sexually Transmitted Infections & HIV
- Tuberculosis
- Unexplained Deaths & Critical Illnesses
- Vaccine-Preventable Diseases
- Vectorborne Diseases
- Viral Respiratory Diseases
- Waterborne Diseases
- Zoonotic & Fungal Diseases
Related Topics
Contact Info
HIV Infection and AIDS
Annual Summary of Reportable Diseases
HIV (human immunodeficiency virus) is the virus that can cause AIDS (acquired immune deficiency syndrome). HIV is most commonly transmitted during anal and vaginal sex, while sharing syringes or equipment to inject drugs or other substances, and less commonly, during pregnancy, childbirth or breastfeeding.
Without treatment, HIV attacks and weakens the immune system, which makes people living with HIV vulnerable to a variety of infections and some cancers. HIV treatment is so effective that people living with HIV can live a long and healthy life, but there is still no vaccine or cure for HIV.
Published 8/15/2025
2023 Highlights
- Two-thirds (66%) of new HIV cases affect communities of color.
- The number of diagnosed people believed to be living with HIV/AIDS in Minnesota is 9,996.
- Twenty-two percent of new HIV diagnoses were among Hispanic people – second only after White people (34%). This is a shift from past years where a majority of new diagnoses were in White and Black/African American populations.
HIV/AIDS incidence in Minnesota remains moderately low. The most recent state-specific incidence rate data from the CDC is from 2022. Data shows that state-specific HIV infection rates ranged from 0.7 per 100,000 population in Vermont to 27.4 per 100,000 in Georgia. Minnesota had the 10th lowest rate (5.4 cases per 100,000 population).
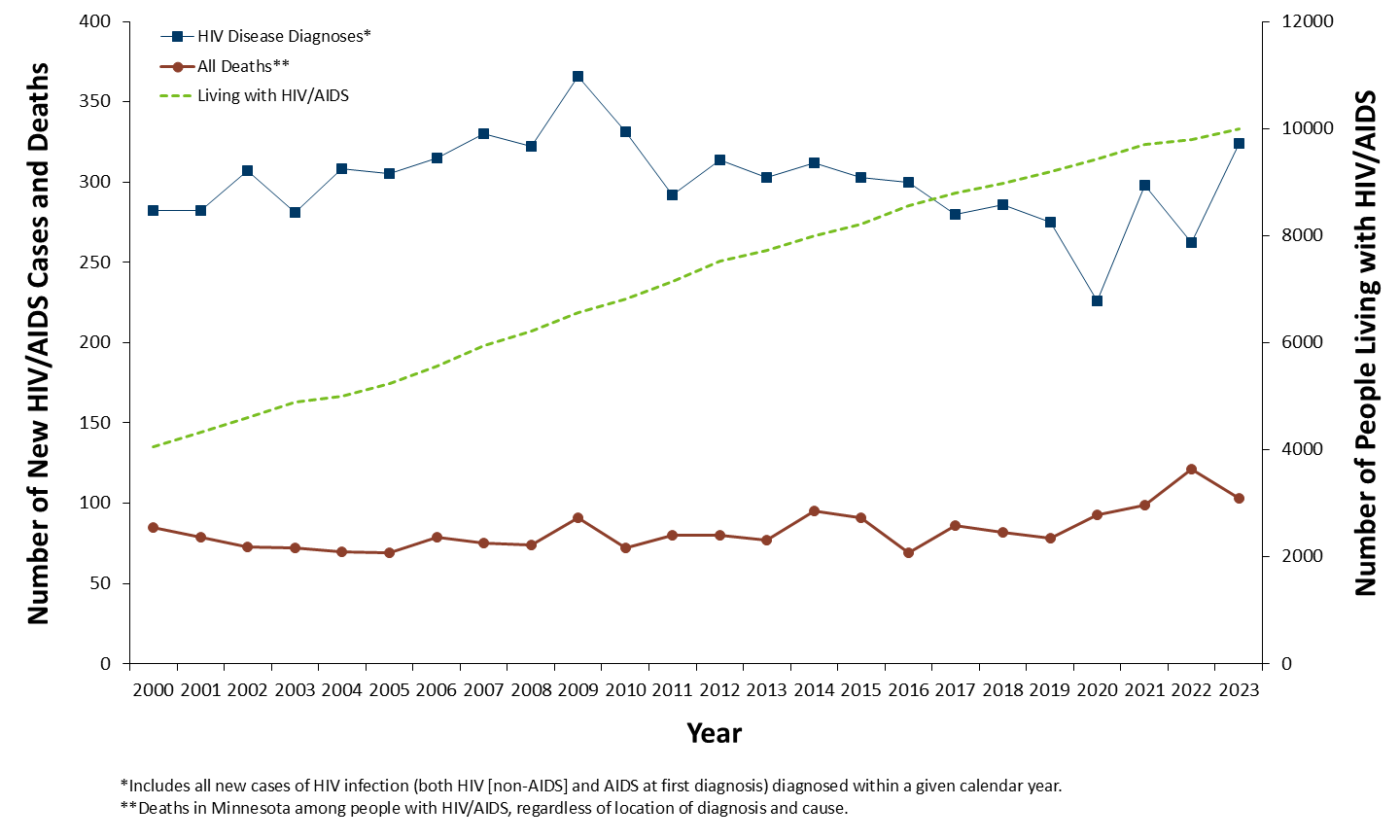
As of December 31, 2023, a cumulative total of 13,216 cases of HIV infection (2,541 AIDS at first diagnosis, and 10,675 HIV [non-AIDS] cases) were reported among Minnesota residents. By the end of 2023, an estimated 9,996 persons with HIV/AIDS were living in Minnesota.
The annual number of HIV/AIDS cases reported in Minnesota increased steadily from 1982 through the early 1990s, reaching a peak of 361 cases in 1992. Beginning in 1996, the annual number of new AIDS diagnoses and deaths declined sharply, primarily due to better antiretroviral therapies. In 2023, the number of cases rose to a new high in the last 10 years: 324 cases. This included 67 new AIDS cases and 103 deaths among persons living with HIV infection in Minnesota were reported.
In 2023, 79% (256/324) of new HIV diagnoses (both HIV [non-AIDS] and AIDS at first diagnosis) occurred in the metropolitan area. In Greater Minnesota, there were 68 cases in 37 counties. HIV infection is most common in areas with higher population densities and poverty levels.
The majority of new HIV infections in Minnesota occurred among males. Trends in the annual number of new HIV infections diagnosed among males differed by race/ethnicity. New infections occurred primarily among white males in the 1980s and early 1990s. Whites still comprise the largest number of HIV infections among males, but the proportion of cases in white males is decreasing. In 2023, there were 94 new infections among white males, comprising 35% of new HIV infections among males. Among black African American males, there were 56 new HIV diagnoses in 2023, making up 20% of new HIV infections among males. Hispanic males (of any race) made up 25% of all cases HIV infections among males.
Females account for an increasing percentage of new HIV infections, from 11% of new infections in 1990 to 18% in 2023. Trends in annual, diagnosed HIV infections among females also differed by race/ethnicity. Early in the epidemic, whites accounted for the majority of newly diagnosed infections. Since 1991, the number of new infections among women of color has exceeded that of white women. In 2023, women of color accounted for 72% of new HIV infections among females in Minnesota. The number of diagnoses among African-born women has been increasing over the past decade. In 2023, the number of new cases among African-born women was 13, accounting for 23% of all new diagnoses among women. In 2023, there were also 13 cases (23%) diagnosed among African American women.
Despite relatively small numbers of cases, HIV/AIDS affects persons of color disproportionately in Minnesota. In 2023, men of color comprised approximately 17% of the male population in Minnesota and 65% of new HIV diagnoses among men. Similarly, persons of color comprised approximately 17% of the female population in Minnesota and 72% of new HIV infections among women. The use of race can be a proxy for other risk factors, such as lower socioeconomic status and education level. Race is not considered a biological cause of disparities in the occurrence of HIV.
Historically, race/ethnicity data for HIV/AIDS in Minnesota has grouped non-African born blacks and black African-born persons together as “black.” In 2001, MDH began analyzing these groups separately, and a marked trend of increasing numbers of new HIV infections among black African-born persons was observed. In 2023, there were 31 new HIV infections reported among black Africans. While black African-born persons comprise about 2% of the state’s population, they accounted for 10% of all HIV infections diagnosed in Minnesota in 2023.
In 2023, there were 131 people diagnosed with HIV who were less than 30 years of age, accounting for 40% of all cases. Most of the cases were among young males, where 45% of male cases were less than 30 years of age and 74% were males younger than 40 years of age.
Since the beginning of the epidemic, male-to-male sex (men who have sex with men; MSM) has been the predominant mode of exposure to HIV reported in Minnesota. In 2023, MSM (including MSM who also inject drugs) accounted for 69% of new diagnoses among men. Injection Drug Use (IDU) was the predominant mode of exposure for women (of those with known exposure).
In the fall of 2019, an outbreak was declared among persons who inject drugs (PWID) diagnosed with HIV in Minnesota. There was a statewide, two-fold increase among PWID with 11 cases in 2018 increasing to 22 cases in 2019. The outbreak area included residents of Hennepin and Ramsey counties, where an alert was indicated among PWID. At the end of 2020, the outbreak included 101 cases. In 2022, the case definition was split into two groups based on molecular data and epidemiological links: Encampment-related and MSM/IDU & IDU-related. At the end of 2023, there were 235 cases (101 encampment-related and 134 MSM/IDU & IDU non-encampment-related)
In the fall of 2020, an alert for the Duluth area was indicated among newly diagnosed HIV infections, after which an outbreak was declared in March 2021. There were 39 cases associated with the outbreak between September 2019 and the end of 2023. Typically, there are from one to five cases of HIV per year in St. Louis County. The health alert also indicated a rise in the number of syphilis cases in the Duluth area. Both declared outbreaks are currently on-going.
HIV perinatal transmission in the United States decreased 90% since the early 1990s. The trend in Minnesota has been similar. While the number of births to HIV-infected women increased nearly 7-fold between 1990 and 2019, with 57 births to pregnant persons in 2023, the rate of perinatal transmission decreased, from 15% in 1994-1996 to 0% over the last 5 years (2019-2023). The last HIV-positive Minnesota birth occurred in 2017.
Archive of HIV Infection and AIDS Annual Summaries
HIV/AIDS incidence in Minnesota remains moderately low. The most recent state-specific incidence rate data from the CDC is from 2020. Data shows that state-specific HIV infection rates ranged from 1.5 per 100,000 population in Montana to 22.1 per 100,000 in Georgia. Minnesota had the 14th lowest rate (4.8 cases per 100,000 population).
As of December 31, 2022, a cumulative total of 12,912 cases of HIV infection (2,468 AIDS at first diagnosis, and 10,444 HIV [non-AIDS] cases) were reported among Minnesota residents. By the end of 2022, an estimated 9,805 persons with HIV/AIDS were living in Minnesota.
The annual number of AIDS cases reported in Minnesota increased steadily from 1982 through the early 1990s, reaching a peak of 361 cases in 1992. Beginning in 1996, the annual number of new AIDS diagnoses and deaths declined sharply, primarily due to better antiretroviral therapies. In 2022, 39 new AIDS cases (Figure 3) and 121 deaths among persons living with HIV infection in Minnesota were reported.
The number of HIV (non-AIDS) diagnoses has varied over the past decade. There was a peak of 280 newly diagnosed HIV (non-AIDS) cases in 2009, and a low of 186 new HIV (non-AIDS) cases reported in 2020. Before 2020, the lowest number of cases reported was 215 new HIV (non-AIDS) cases, reported in 2017.
In 2022, 76% (200/262) of new HIV diagnoses (both HIV [non-AIDS] and AIDS at first diagnosis) occurred in the metropolitan area. In Greater Minnesota there were 62 cases in 23 of 80 counties. HIV infection is most common in areas with higher population densities and poverty levels.
The majority of new HIV infections in Minnesota occurred among males. Trends in the annual number of new HIV infections diagnosed among males differed by race/ethnicity. New infections occurred primarily among white males in the 1980s and early 1990s. Whites still comprise the largest number of HIV infections among males, but the proportion of cases in white males is decreasing. In 2022, there were 79 new infections among white males, comprising 37% of new HIV infections among males. Among black African American males, there were 62 new HIV diagnoses in 2022, which is about a third of new HIV infections among males (29%). Among Hispanic males of any race and black African-born males, there were 35 and 13 new HIV infections in 2022, respectively.
Females account for an increasing percentage of new HIV infections, from 11% of new infections in 1990 to 19% in 2022. Trends in annual, diagnosed HIV infections among females also differed by race/ethnicity. Early in the epidemic, whites accounted for the majority of newly diagnosed infections. Since 1991, the number of new infections among women of color has exceeded that of white women. In 2022, women of color accounted for 71% of new HIV infections among females in Minnesota. The number of diagnoses among African-born women has been increasing over the past decade. In 2022, the number of new cases among African-born women was 10, accounting for 20% of all new diagnoses among women. In 2022, there were 15 cases (29%) diagnosed among African American women.
Despite relatively small numbers of cases, HIV/AIDS affects persons of color disproportionately in Minnesota. In 2022, men of color comprised approximately 17% of the male population in Minnesota and 60% of new HIV diagnoses among men. Similarly, persons of color comprised approximately 17% of the female population in Minnesota and 71% of new HIV infections among women. The use of race can be a proxy for other risk factors, such as lower socioeconomic status and education level. Race is not considered a biological cause of disparities in the occurrence of HIV.
Historically, race/ethnicity data for HIV/AIDS in Minnesota has grouped non-African born blacks and black African-born persons together as “black.” In 2001, MDH began analyzing these groups separately, and a marked trend of increasing numbers of new HIV infections among black African-born persons was observed. In 2022, there were 23 new HIV infections reported among black Africans. While black African-born persons comprise about 2% of the state’s population, they accounted for 9% of all HIV infections diagnosed in Minnesota in 2022.
In 2022, there were 105 people diagnosed with HIV who were less than 30 years of age, accounting for 40% of all cases. Most of the cases were among young males, where 45% of male cases were less than 30 years of age and 72% were males younger than 40 years of age.
Since the beginning of the epidemic, male-to-male sex (men who have sex with men; MSM) has been the predominant mode of exposure to HIV reported in Minnesota. In 2022, MSM (including MSM who also inject drugs) accounted for 60% of new diagnoses among men. Injection Drug Use (IDU) was the predominant mode of exposure for women (of those with known exposure).
In the fall of 2019, an outbreak was declared among persons who inject drugs (PWID) diagnosed with HIV in Minnesota. There was a statewide, two-fold increase among PWID with 11 cases in 2018 increasing to 22 cases in 2019. The outbreak area included residents of Hennepin and Ramsey counties, where an alert was indicated among PWID. At the end of 2020, the outbreak included 101 cases. In 2022, the case definition was split into two groups based on molecular data and epidemiological links: Encampment-related and MSM/ IDU & IDU-related. At the end of 2022, there were 168 cases (73 encampment-related and 95 MSM/IDU & IDU non-encampment-related).
In the fall of 2020, an alert for the Duluth area was indicated among newly diagnosed HIV infections, after which an outbreak was declared in March 2021. There were 35 cases associated with the outbreak between September 2019 and the end of 2023. Typically, there are from one to five cases of HIV per year in St. Louis County. The health alert also indicated a rise in the number of syphilis cases in the Duluth area. Both declared outbreaks are currently on-going.
HIV perinatal transmission in the United States decreased 90% since the early 1990s. The trend in Minnesota has been similar. While the number of births to HIV-infected women increased nearly 7-fold between 1990 and 2019, with 37 births to pregnant persons in 2022, the rate of perinatal transmission decreased, from 15% in 1994-1996 to 0% over the last 5 years (2018-2022). The last HIV-positive Minnesota birth occurred in 2017.
- For up to date information see: HIV/AIDS
HHIV/AIDS incidence in Minnesota remains moderately low. The most state-specific recent rate data is from 2020, which shows that state-specific HIV infection rates ranged from 1.5 per 100,000 population in Montana to 22.1 per 100,000 in Georgia. Minnesota had the 14th lowest rate (4.8 cases per 100,000 population).
As of December 31, 2021, a cumulative total of 12,643 cases of HIV infection (2,418 AIDS at first diagnosis, and 10,225 HIV [non-AIDS] cases) were reported among Minnesota residents. By the end of 2021, an estimated 9,696 persons with HIV/AIDS were living in Minnesota.
The annual number of AIDS cases reported in Minnesota increased steadily from 1982 through the early 1990s, reaching a peak of 361 cases in 1992. Beginning in 1996, the annual number of new AIDS diagnoses and deaths declined sharply, primarily due to better antiretroviral therapies. In 2021, 81 new AIDS cases (Figure 4) and 99 deaths among persons living with HIV infection in Minnesota were reported.
The number of HIV (non-AIDS) diagnoses has varied over the past decade. There was a peak of 278 newly diagnosed HIV (non-AIDS) cases in 2009, and a low of 183 new HIV (non-AIDS) cases reported in 2020. Before 2020, the lowest number of cases reported was 215 new HIV (non-AIDS) cases, reported in 2017.
In 2021, 74% (222/298) of new HIV diagnoses (both HIV [non-AIDS] and AIDS at first diagnosis) occurred in the metropolitan area. In Greater Minnesota there were 76 cases in 29 of 80 counties. HIV infection is most common in areas with higher population densities and greater poverty.
The majority of new HIV infections in Minnesota occur among males. Trends in the annual number of new HIV infections diagnosed among males differ by race/ethnicity. New infections occurred primarily among white males in the 1980s and early 1990s. Whites still comprise the largest number of HIV infections among males, but the proportion of cases accounted for by white males account is decreasing. In 2021, there were 87 new infections among white males, which is 37% of new HIV infections among males. Among black African American males, there were 68 new HIV diagnoses in 2021, which is about a third of new HIV infections among males (29%). Among Hispanic males of any race and black African-born males, there were 41 and 21 new HIV infections in 2021, respectively.
Females account for an increasing percentage of new HIV infections, from 11% of new infections in 1990 to 21% in 2021. Trends in HIV infections diagnosed annually among females also differ by race/ ethnicity. Early in the epidemic, whites accounted for the majority of newly diagnosed infections. Since 1991, the number of new infections among women of color has exceeded that of white women.
In 2021, women of color accounted for 73% of new HIV infections among females in Minnesota. The number of diagnoses among African-born women has been increasing over the past decade. In 2021, the number of new cases among African-born women was 25, accounting for 39% of all new diagnoses among women. In 2021, there were 10 cases (16%) diagnosed among African American women.
Despite relatively small numbers of cases, HIV/AIDS affects persons of color disproportionately in Minnesota. In 2021, men of color comprised approximately 17% of the male population in Minnesota and 61% of new HIV diagnoses among men. Similarly, persons of color comprised approximately 17% of the female population in Minnesota and 73% of new HIV infections among women. It bears noting the use of race can be a proxy for other risk factors, including lower socioeconomic status and education. Race is not considered a biological cause of disparities in the occurrence of HIV.
Historically, race/ethnicity data for HIV/AIDS in Minnesota have grouped non-African born blacks and black African-born persons together as “black.” In 2001, MDH began analyzing these groups separately, and a marked trend of increasing numbers of new HIV infections among black African-born persons was observed. In 2021, there were 46 new HIV infections reported among black Africans. While black African-born persons comprise about 2% of the state’s population, they accounted for 15% of all HIV infections diagnosed in Minnesota in 2021.
In 2021, there were 88 diagnosed with HIV less than 30 years of age, accounting for 34% of all cases. Most of the cases were among young males, where 87% of cases were less than 30 years of age.
Since the beginning of the epidemic, male-to-male sex (men who have sex with men; MSM) has been the predominant mode of exposure to HIV reported in Minnesota. In 2021, MSM (including MSM who also inject drugs) accounted for 53% of new diagnoses among men. IDU was the predominant mode of exposure for women (of those with known exposure).
In the fall of 2019, an outbreak was declared among persons who inject drugs (PWID) diagnosed with HIV in Minnesota. Statewide there was a two-fold increase among PWID with 11 cases in 2018 increasing to 22 cases in 2019. The outbreak area included residents of Hennepin and Ramsey counties, where an alert was indicated among PWID. At the end of 2020, the outbreak included 101 cases. Persons likely to be at high risk for HIV infection include sex partners or syringe-sharing partners of people known to be living with HIV, PWID and their sex partners and needle sharing partners, persons who exchange sex for income or other items they need, and persons who experienced or are currently experiencing homelessness.
In the fall of 2020, an alert for the Duluth area was indicated among newly diagnosed HIV infections, after which an outbreak was declared in March 2021. There were 23 cases associated with the outbreak between September 2019 and the beginning of 2021. Typically, there are from one to five cases of HIV per year in St. Louis County. The health alert also indicated a rise in the number of syphilis cases in the Duluth area. Both declared outbreaks are currently on-going.
HIV perinatal transmission in the United States decreased 90% since the early 1990s. The trend in Minnesota has been similar. While the number of births to HIV-infected women increased nearly 7-fold between 1990 and 2019, with 60 births to pregnant persons in 2021, the rate of perinatal transmission decreased, from 15% in 1994-1996 to 0% over the last 4 years (2018-2021), with the last HIV-positive Minnesota birth in 2017.
- For up to date information see: HIV/AIDS
HIV/AIDS incidence in Minnesota remains moderately low. In 2018, state-specific HIV infection rates ranged from 2.5 per 100,000 population in Wyoming to 29.2 per 100,000 in Georgia. Minnesota had the 14th lowest rate (6.1 cases per 100,000 population). In 2018, state-specific AIDS diagnosis rates ranged from 0.4 per 100,000 persons in Wyoming to 13.9 per 100,000 population in Georgia. Minnesota had the 15th lowest rate (2.5 cases per 100,000 population).
As of December 31, 2020, a cumulative total of 12,339 cases of HIV infection (2,355 AIDS at first diagnosis, and 9,987 HIV [non-AIDS] cases) were reported among Minnesota residents. By the end of 2020, an estimated 9,422 persons with HIV/AIDS were living in Minnesota.
The annual number of AIDS cases reported in Minnesota increased steadily from 1982 through the early 1990s, reaching a peak of 361 cases in 1992. Beginning in 1996, the annual number of new AIDS diagnoses and deaths declined sharply, primarily due to better antiretroviral therapies. In 2020, 68 new AIDS cases (Figure 3) and 93 deaths among persons living with HIV infection in Minnesota were reported.
The number of HIV (non-AIDS) diagnoses has varied over the past decade (Figure 3). There was a peak of 278 newly diagnosed HIV (non-AIDS) cases in 2009, and a low of 183 new HIV (non-AIDS) cases reported in 2020. Before 2020, the lowest number of cases reported was 215 new HIV (non-AIDS) cases reported in 2017.
In 2020, 76% (173/226) of new HIV diagnoses (both HIV [non-AIDS] and AIDS at first diagnosis) occurred in the metropolitan area. In Greater Minnesota there were 53 cases in 28 of 80 counties. HIV infection is most common in areas with higher population densities and greater poverty.
The majority of new HIV infections in Minnesota occur among males. Trends in the annual number of new HIV infections diagnosed among males differ by race/ethnicity. New infections occurred primarily among white males in the 1980s and early 1990s. Whites still comprise the largest number of HIV infections among males, but the proportion of cases that white males account for is decreasing. In 2020, there were 65 new infections among white males, which is 34% of new HIV infections among males. Among black African American males, there were 61 new HIV diagnoses in 2020, which is about a third of new HIV infections among males (32%). Among Hispanic males of any race and black African-born males, there were 30 and 14 new HIV infections in 2020 respectively.
Females account for an increasing percentage of new HIV infections, from 11% of new infections in 1990 to 20% in 2020. Trends in HIV infections diagnosed annually among females also differ by race/ethnicity. Early in the epidemic, whites accounted for the majority of newly diagnosed infections. Since 1991, the number of new infections among women of color has exceeded that of white women.
In 2020, women of color accounted for 81% of new HIV infections among females in Minnesota. The number of diagnoses among African-born women has been increasing over the past decade. In 2020, the number of new cases among African-born women was 11, accounting for 30% of all new diagnoses among women. In 2020, there were 11 cases (30%) diagnosed among African American women.
Despite relatively small numbers of cases, HIV/AIDS affects persons of color disproportionately in Minnesota. In 2020, men of color comprised approximately 17% of the male population in Minnesota and 66% of new HIV diagnoses among men. Similarly, persons of color comprised approximately 13% of the female population in Minnesota and 81% of new HIV infections among women. It bears noting the use of race can be a proxy for other risk factors, including lower socioeconomic status and education, and race is not considered a biological cause of disparities in the occurrence of HIV.
In 2020, there were 88 diagnosed with HIV less than 30 years of age, accounting for 39% of all cases. Most of the cases were among young males where 89% of cases less than 30 years were male.
Since the beginning of the epidemic, male-to-male sex (men who have sex with men; MSM) has been the predominant mode of exposure to HIV reported in Minnesota. In 2020, MSM (including MSM who also inject drugs) accounted for 55% of new diagnoses among men. Heterosexual contact with a partner who has or is at increased risk of HIV infection is the predominant mode of exposure to HIV for women.
In the fall of 2019, an outbreak was declared among persons who inject drugs (PWID) diagnosed with HIV in Minnesota. Statewide there was a two-fold increase among PWID with 11 cases in 2018 increasing to 22 cases in 2019. The outbreak area includes residents of Hennepin and Ramsey counties where an alert was indicated among PWID. At the end of 2020, the outbreak included 27 cases. Persons likely to be at high risk for HIV infection include sex partners or syringe-sharing partners of people known to be living with HIV, PWID and their sex partners and needle sharing partners, persons who exchange sex for income or other items they need, and persons who experienced or are currently experiencing homelessness.
In fall 2020, an alert for the Duluth area was indicated among newly diagnosed HIV infections in which an outbreak was declared in March 2021. There have been 13 cases associated with the outbreak between September 2019 and February 2021 when the outbreak was declared. Typically, there are 1 to 5 cases of HIV annually in St. Louis County. The health alert also indicated a rise in the number of syphilis cases in the Duluth area. Both declared outbreaks are currently on-going.
Historically, race/ethnicity data for HIV/AIDS in Minnesota have grouped non-African born blacks and black African-born persons together as “black.” In 2001, MDH began analyzing these groups separately, and a marked trend of increasing numbers of new HIV infections among black African-born persons was observed. In 2020, there were 25 new HIV infections reported among black Africans. While black African-born persons comprise less than 1% of the state’s population, they accounted for 11% of all HIV infections diagnosed in Minnesota in 2020.
HIV perinatal transmission in the United States decreased 90% since the early 1990s. The trend in Minnesota has been similar. While the number of births to HIV-infected women increased nearly 7-fold between 1990 and 2019, with 42 births to pregnant persons in 2020, the rate of perinatal transmission decreased, from 15% in 1994-1996 to 0% over the last 3 years (2018-2020), with the last HIV-positive Minnesota birth in 2017.
- For up to date information see: HIV/AIDS
HIV/AIDS incidence in Minnesota remains moderately low. In 2018, state-specific HIV infection rates ranged from 2.5 per 100,000 population in Wyoming to 28.6 per 100,000 in Georgia. Minnesota had the 14th lowest rate (6.2 cases per 100,000 population). In 2018, state-specific AIDS diagnosis rates ranged from 0.3 per 100,000 persons in Wyoming to 11.6 per 100,000 population in Georgia. Minnesota had the 15th lowest rate (2.1 cases per 100,000 population).
As of December 31, 2019, 2,112 cases of HIV infection (2,308 AIDS at first diagnosis, and 9,804 HIV [non-AIDS] cases) were reported among Minnesota residents. By the end of 2019, an estimated 9,193 persons with HIV/AIDS were living in Minnesota.
The annual number of AIDS cases reported in Minnesota increased steadily from 1982 through the early 1990s, reaching a peak of 361 cases in 1992. Beginning in 1996, the annual number of new AIDS diagnoses and deaths declined sharply, primarily due to better antiretroviral therapies. In 2019, 111 new AIDS cases (Figure 4) and 76 deaths among persons living with HIV infection in Minnesota were reported.
The number of HIV (non-AIDS) diagnoses has varied over the past decade. There was a peak of 278 newly diagnosed HIV (non-AIDS) cases in 2009, and a low of 215 new HIV (non-AIDS) cases reported in 2017, which is slightly lower than 219 cases reported in 2019.
In 2019, 81% (222/275) of new HIV diagnoses (both HIV [non-AIDS] and AIDS at first diagnosis) occurred in the metropolitan area. In greater Minnesota there were 52 cases in 31 of 78 counties. HIV infection is most common in areas with higher population densities and greater poverty.
The majority of new HIV infections in Minnesota occur among males. Trends in the annual number of new HIV infections diagnosed among males differ by race/ethnicity. New infections occurred primarily among white males in the 1980s and early 1990s. Whites still comprise the largest number of HIV infections among males, but the proportion of cases that white males account for is decreasing. In 2019, there were 84 new infections among white males, which is slightly less than half of new HIV infections among males (42%). Among black African American males, there were 51 new HIV diagnoses in 2019, which is about a quarter of new HIV infections among males (26%). Among Hispanic males of any race and black African-born males, there were 33 and 12 new HIV infections in 2019 respectively.
Females account for an increasing percentage of new HIV infections, from 11% of new infections in 1990 to 28% in 2019. Trends in HIV infections diagnosed annually among females also differ by race/ethnicity. Early in the epidemic, whites accounted for the majority of newly diagnosed infections. Since 1991, the number of new infections among women of color has exceeded that of white women.
In 2019, women of color accounted for 68% of new HIV infections among females in Minnesota. The number of diagnoses among African-born women has been increasing over the past decade. In 2019, the number of new cases among African-born women was 25, accounting for 33% of all new diagnoses among women. In 2019, there were 11 cases (14%) diagnosed among African American women.
Despite relatively small numbers of cases, HIV/AIDS affects persons of color disproportionately in Minnesota. In 2019, men of color comprised approximately 17% of the male population in Minnesota and 58% of new HIV diagnoses among men. Similarly, persons of color comprised approximately 13% of the female population in Minnesota and 68% of new HIV infections among women. The use of race can be a proxy for other risk factors, including lower socioeconomic status and education, and race is not considered a biological cause of disparities in the occurrence of HIV.
Historically, race/ethnicity data for HIV/AIDS in Minnesota have grouped non-African born blacks and black African-born persons together as “black.” In 2001, MDH began analyzing these groups separately, and a marked trend of increasing numbers of new HIV infections among black African-born persons was observed. In 2019, there were 37 new HIV infections reported among black Africans. While black African-born persons comprise less than 1% of the state’s population, they accounted for 14% of all HIV infections diagnosed in Minnesota in 2019.
In 2019, there were 111 diagnosed with HIV less than 30 years of age, accounting for 40% of all cases. Most of the cases were among young males where 82% of cases less than 30 years were male.
Since the beginning of the epidemic, male-to-male sex (men who have sex with men; MSM) has been the predominant mode of exposure to HIV reported in Minnesota. In 2019, MSM (including MSM who also inject drugs) accounted for 67% of new diagnoses among men. Heterosexual contact with a partner who has or is at increased risk of HIV infection is the predominant mode of exposure to HIV for women.
In the fall of 2019, an outbreak was declared among persons who inject drugs (PWID) diagnosed with HIV in Minnesota. Statewide there was a two-fold increase among PWID with 11 cases in 2018 increasing to 22 cases in 2019. The outbreak area includes residents of Hennepin and Ramsey counties where about three quarters of the statewide cases are located (16, 72%). Persons likely to be at high risk for HIV infection include sex partners or syringe-sharing partners of people known to be living with HIV, PWID and their sex partners and needle sharing partners, persons who exchange sex for income or other items they need, and persons who experienced or are currently experiencing homelessness.
HIV perinatal transmission in the United States decreased 90% since the early 1990s. The trend in Minnesota has been similar. While the number of births to HIV-infected women increased nearly 7-fold between 1990 and 2018, with 57 births to pregnant persons in 2019, the rate of perinatal transmission decreased, from 15% in 1994-1996 to 0.6% over the last 3 years (2017- 2019), with 1 HIV-positive birth in 2017.
- Find up to date information at>> HIV/AIDS
HIV/AIDS incidence in Minnesota remains moderately low. In 2017, state-specific HIV infection rates ranged from 2.1 per 100,000 population in Wyoming to 30.0 per 100,000 in Georgia. Minnesota had the 16th lowest rate (6.0 cases per 100,000 population). In 2017, state specific AIDS diagnosis rates ranged from 0.9 per 100,000 persons in New Hampshire to 12.5 per 100,000 population in Georgia. Minnesota had the 16th lowest rate (2.6 cases per 100,000 population).
As of December 31, 2018, a cumulative total of 11,852 cases of HIV infection (2,267 AIDS at first diagnosis, and 9,585 HIV [non-AIDS] cases) were reported among Minnesota residents. By the end of 2018, an estimated 8,981 persons with HIV/AIDS were living in Minnesota.
The annual number of AIDS cases reported in Minnesota increased steadily from 1982 through the early 1990s, reaching a peak of 361 cases in 1992. Beginning in 1996, the annual number of new AIDS diagnoses and deaths declined sharply, primarily due to better antiretroviral therapies. In 2018, 116 new AIDS cases (Figure 4) and 82 deaths among persons living with HIV infection in Minnesota were reported.
The number of HIV (non-AIDS) diagnoses has varied over the past decade. There was a peak of 278 newly diagnosed HIV (non-AIDS) cases in 2009, and a low of 215 new HIV (non-AIDS) cases reported in 2017, which is lower than 228 cases reported in 2018.
In 2018, 77% (221/286) of new HIV diagnoses (both HIV [non-AIDS] and AIDS at first diagnosis) occurred in the metropolitan area. In Greater Minnesota there were 65 cases in 35 counties. HIV infection is most common in areas with higher population densities and greater poverty.
The majority of new HIV infections in Minnesota occur among males. Trends in the annual number of new HIV infections diagnosed among males differ by race/ethnicity. New infections occurred primarily among white males in the 1980s and early 1990s. Whites still comprise the largest number of HIV infections among males, but the proportion of cases that white males account for is decreasing. In 2018, there were 93 new infections among white males, which is slightly less than half of new HIV infections among males (43%). Among black African American males, there were 49 new HIV diagnoses in 2018, which is about a quarter of new HIV infections among males (23%). Among Hispanic males of any race and black African-born males, there were 34 and 23 new HIV infections in 2018 respectively.
Females account for an increasing percentage of new HIV infections, from 11% of new infections in 1990 to 24% in 2018. Trends in HIV infections diagnosed annually among females also differ by race/ethnicity. Early in the epidemic, whites accounted for the majority of newly diagnosed infections. Since 1991, the number of new infections among women of color has exceeded that of white women.
In 2018, women of color accounted for 69% of new HIV infections among females in Minnesota. The number of diagnoses among African-born women has been increasing over the past decade. In 2018, the number of new cases among African-born women was 25, accounting for 37% of all new diagnoses among women. In 2018, there were 13 cases (19%) diagnosed among African American women.
Despite relatively small numbers of cases, HIV/AIDS affects persons of color disproportionately in Minnesota. In 2018, men of color comprised approximately 17% of the male population in Minnesota and 57% of new HIV diagnoses among men.
Similarly, persons of color comprised approximately 13% of the female population in Minnesota and 69% of new HIV infections among women. It bears noting the use of race can be a proxy for other risk factors, including lower socioeconomic status and education, and race is not considered a biological cause of disparities in the occurrence of HIV.
In 2018, there were 103 diagnosed with HIV less than 30 years of age, accounting for 36% of all cases. Most of these cases were among young males; 83% of cases less than 30 years were male. The average age at diagnosis in 2018 was 34 years for males and 38 years for females. A population of concern for HIV infection is adolescents and young adults (13-24 years). The number of new HIV infections among males in this age group has remained higher than new diagnoses among females since 1999, with 33 cases reported in 2018, which is lower than 47 cases reported in 2017. The number of new HIV infections among adolescent females has remained relatively consistent over time; in 2018 there were 5 cases. From 2016 to 2018, the majority (66%) of new infections among male adolescents and young adults were among youth of color, with young black African American males accounting for 34% of cases among young males of color. During the same period, young women of color accounted for 75% of the cases diagnosed, with young black African American women accounting for 43% of cases among young women of color.
Since the beginning of the epidemic, male-to-male sex (men who have sex with men; MSM) has been the predominant mode of exposure to HIV reported in Minnesota. In 2018, MSM (including MSM who also inject drugs) accounted for 71% of new diagnoses among men. Heterosexual contact with a partner who has or is at increased risk of HIV infection is the predominant mode of exposure to HIV for women.
among women was attributed to heterosexual exposure. The number of cases among people who inject drugs (IDU and MSM/IDU mode of exposure) has increased slightly over the past 3 years with 32 cases in 2018 compared to 26 cases in 2017, which indicates a continued pattern of increased HIV infection among people who inject drugs in the state.
Historically, race/ethnicity data for HIV/AIDS in Minnesota have grouped non-African born blacks and black African-born persons together as “black.” In 2001, MDH began analyzing these groups separately, and a marked trend of increasing numbers of new HIV infections among black African-born persons was observed. In 2018, there were 48 new HIV infections reported among black Africans. While black African-born persons comprise less than 1% of the state’s population, they accounted for 17% of all HIV infections diagnosed in Minnesota in 2018.
HIV perinatal transmission in the United States decreased 90% since the early 1990s. The trend in Minnesota has been similar. While the number of births to HIV-infected women increased nearly 7-fold between 1990 and 2018, with 65 births to pregnant persons in 2018, the rate of perinatal transmission decreased, from 15% in 1994-1996 to 0.6% over the last 3 years (2016- 2018), with 1 HIV-positive birth in 2017.
- For up to date information see>> HIV/AIDS
- Archive of Annual Summary of Communicable Diseases Reported to the Minnesota Department of Health
Archive of past summaries (years prior to 2023 are available as PDFs).
