Refugee Health
- Refugee Health Home
- About
- Statistics
- Stories from Minnesota Refugees
- Refugee Health Assessment Coordination
- For Resettlement Agencies
- For LPH and Health Care Providers
- For Community Sponsors
- Directories for Organizations Serving Diverse Communities
- Health Education Materials
- Trainings and Events
- Center of Excellence in Newcomer Health
Spotlight
Newcomer Skin Conditions Guidance for Health Professionals
Minnesota has welcomed an increasing number of newcomers who have traveled here via the southern border from a variety of regions, including Central and South America and West Africa. Many of these newcomers may be at risk for dermatological diseases due to poor conditions in their country of residence or during their journey, such as household overcrowding, inadequate sanitation facilities, environmental exposures, and a lack of access to health care. In addition, some may present with vaccine-preventable diseases and neglected tropical diseases with skin manifestations that may not be immediately recognized. This resource is intended as a guide to possible skin conditions that may be encountered in primary care settings where newcomers are screened and receive care.
Identification of rashes on non-white skin
Many dermatological teaching and reference resources have historically lacked illustrations of common skin findings on black and brown skin. Some rashes, particularly those with erythema as a typical finding, may be more difficult to appreciate on darker skin. For example, eczema flare-ups may appear grayish, violaceous, or dark brown instead of pink or red. Areas of hyperpigmentation may be mistaken for post-inflammatory hyperpigmentation changes instead of areas of active inflammation.
 | Lichenification and hyperpigmentation on the knees in skin of color due to atopic eczema Source: DermNet: Atopic dermatitis |
 | Papules in the interdigital web space due to scabies Source: CDC: Public Health Image Library |
The World Health Organization (WHO) has created a training guide for recognizing neglected tropical diseases of the skin for front-line health workers with multiple images of both common skin conditions (e.g., acne, atopic eczema, impetigo, psoriasis, scabies) and tropical diseases (e.g., Buruli ulcer, cutaneous leishmaniasis, lymphatic filariasis, onchocerciasis) on non-white skin. The WHO guide is available for download as a handbook (Recognizing neglected tropical diseases through changes on the skin: a training guide for front-line health workers) and as an interactive mobile app for both Android and iOS (named “Skin NTDs App” on the Google Play and Apple App Store). Both handbook and app are available free of charge.
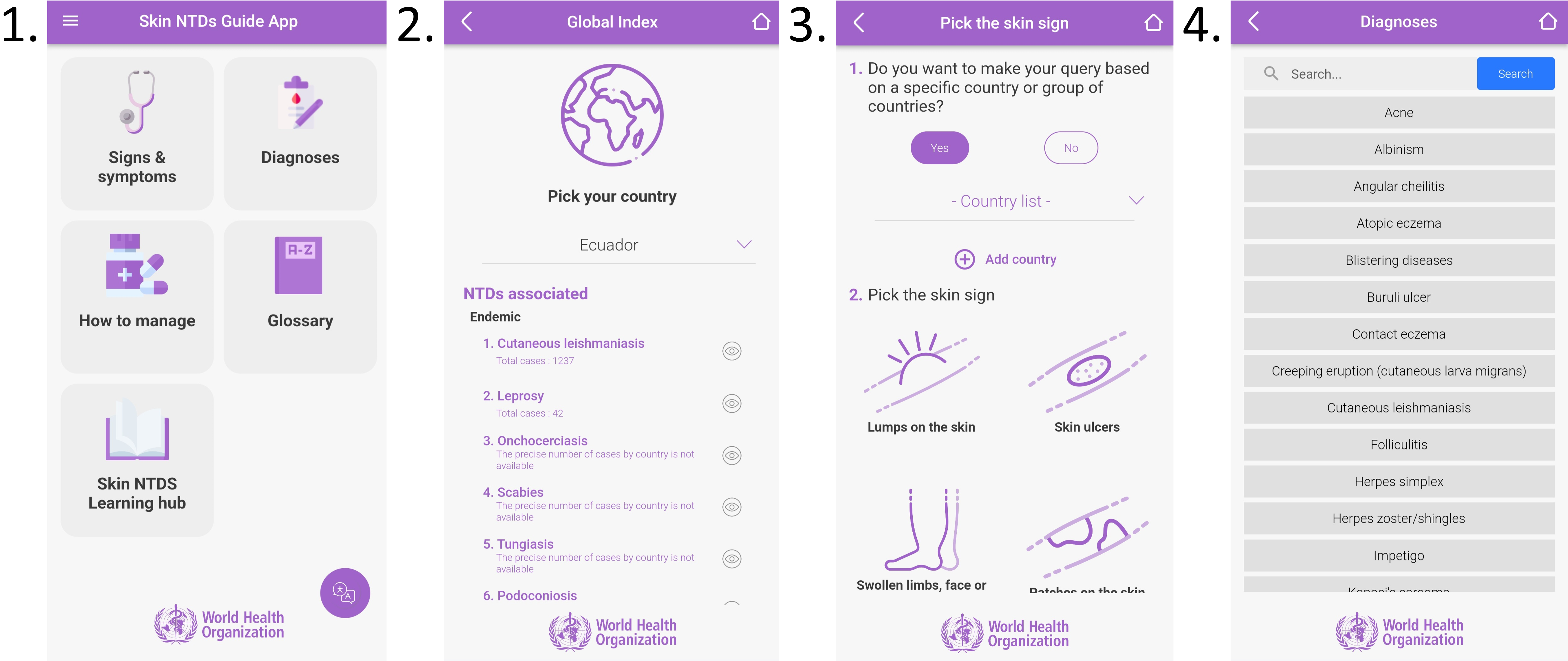
1 WHO Skin NTDs Guide App: Homepage
2 WHO Skin NTDs Guide App: Searchable list of conditions by country
3 WHO Skin NTDs Guide App: Skin conditions diagnosis tool
4 WHO Skin NTDs Guide App: List of skin diagnoses
The Inclusive Skin Color Project at the University of California San Francisco (UCSF) also maintains a list of open access image banks, atlases, and other resources aimed at increasing access to representative and inclusive images of skin findings.
General skin disorders
This is not a comprehensive list of all skin conditions that can occur. Individual conditions may present in ways not listed here or in atypical forms. Providers should refer to additional resources linked for information on diagnosis and treatment, and the references cited above for pictures of the conditions.
- Scabies
Intensely itchy papules on sides or webs of fingers, wrists, trunk, knees and/or feet
MDH: Scabies - Measles
Maculopapular rash starting on face and spreading downward
MDH: Measles (Rubeola) - Varicella
Scattered itchy vesicles in different stages of development
MDH: Varicella (Chickenpox) - Meningococcal disease
Non-blanching petechial rash associated with systemic illness (fever, shock)
*MEDICAL EMERGENCY*
MDH: Meningococcal Disease (Neisseria meningitidis, "Bacterial Meningitis") - Impetigo
Erythematous papules with crusting around nose and mouth in children
CDC: About Impetigo - Tinea ("ringworm")
Multiple variations affecting skin and nails
MedlinePlus: Ringworm - Herpes simplex
Clusters of small, painful, recurring vesicles progressing to ulcers around mouth or genitals
WHO: Herpes Simplex Virus - Lyme disease
Expanding circular erythematous rash, usually not painful or itchy
MDH: Lyme Disease (Borrelia burgdorferi)
- Atopic dermatitis (eczema)
Itchy erythematous papules with dry skin on antecubital and popliteal fossae, hands, wrists, ankles, neck
AAFP: Atopic Dermatitis: Diagnosis and Treatment - Contact dermatitis (allergic, irritant)
Well-demarcated itchy eruption localized to area of skin in contact with allergen or irritant
AAFP: Diagnosis and Management of Contact Dermatitis ( - Psoriasis
Scaly symmetric well-demarcated plaques on scalp, extensor elbows, knees, and gluteal cleft
AAFP: Psoriasis
- Skin cancer
Any new growth, non-healing sore, or change in an existing mole or freckle
CDC: Skin Cancer
Skin disorders endemic to regions outside the U.S.
This is not a comprehensive list of all skin conditions that can occur. Individual conditions may present in ways not listed here or in atypical forms. Providers should refer to additional resources linked for information on diagnosis and treatment.
- Cutaneous leishmaniasis
Chronic nodule or ulcer on exposed skin location, usually painless, with well-defined, indurated border
CDC: About Leishmaniasis - Cutaneous larva migrans
Intensely itchy, erythematous, serpiginous tracks in lower extremities or buttocks following exposure to contaminated soil or sand (e.g., walking barefoot)
CDC DPDx: Hookworm (Extraintestinal) - Myiasis
Slowly growing nodule(s) containing fly larva following insect bite
CDC: About Myiasis - Buruli ulcer
Chronic progressive ulcer with undermined edges, often painless, often lower limbs
WHO: Buruli ulcer (Mycobacterium ulcerans infection) - Onchocerciasis
Subcutaneous nodules over bony prominences, pruritic inflammatory papules or plaques, depigmentation
WHO: Onchocerciasis - Yaws
Large wart-like lesion progressing to ulceration and secondary nodules on fingers and long bones
WHO: Yaws - Mycetoma (Madura foot)
Progressive non-healing ulcer of foot with nodules and draining sinuses
WHO: Mycetoma - Leprosy
One or more hypopigmented or reddish anesthetic skin patch(es) with thickened peripheral nerve(s)
WHO: Leprosy
Torture, sexual and gender-based violence, and human trafficking and exploitation
Refugees and asylees are at higher risk of having experienced torture and sexual and gender-based violence (SGBV) as well as human trafficking (sex and labor) of all genders. Providers should be aware that both acute and chronic skin lesions, including abrasions, bruises, scars, puncture wounds, burns, skeletal deformities, tattoos, or brands, can represent sequelae of torture, SGBV, or human trafficking and exploitation. Documentation of these findings in the medical record can help to support an individual’s claim of asylum. More information is available at MDH: Newcomer Survivors of Trauma Guidance for Health Professionals, as well as The Center for Victims of Torture and Heal Torture.
